Blepharitis
Blepharitis – Written by Dr Alexis Ceecee Britten-Jones, B Optom (Hons), PhD.
What is blepharitis?
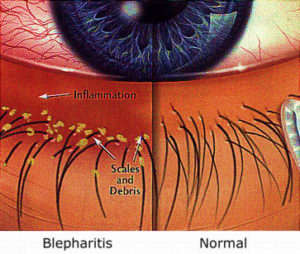
Blepharitis is an inflammation of the eyelids and eyelid margins. The eyelids may become irritated, swollen, and itchy. Blepharitis can also cause dandruff-like flakes at the base of the eyelashes and a crusty material or sticky discharge that causes the eyelids to stick together during sleep.
Blepharitis is a common eye condition. It can cause irritation and discomfort, but it usually does not cause any significant changes to vision.
This overview will cover the public health problem of blepharitis, the different types of blepharitis, its causes, its common signs and symptoms, how it is diagnosed, its treatment options, as well as how it might be prevented.
How many people are affected by blepharitis?
Blepharitis is one of the most common eye conditions reported in eyecare settings. It has been reported in up to one in two people attending eye examinations [1]. The exact number of people that have blepharitis is hard to estimate, because blepharitis is often reported alongside other conditions that also cause inflammation in the eye. However, approximately 50-70% of people who report symptoms of dry eye disease have been found to have blepharitis [2], and dry eye disease is estimated to affect between 14-33% of the world’s population [3].
Blepharitis can affect people of all ages, gender, and ethnicities, but it is more common in people over 50 years of age, and the risk of developing blepharitis increases as a person gets older [4].
Although blepharitis primarily affects adults, it can also happen in children. In children, the inflammation around the eyelids often occurs with redness and infections in other superficial tissues that cover the eye, in a condition called blepharoconjunctivitis [5].
Types of blepharitis
There are two types of blepharitis:
- Anterior blepharitis affects the outer part of the eyelids, the eyelash follicles, and the base of the eyelashes. Anterior blepharitis causes redness along the lid margins and flaky crusts along the base of the eyelashes
- Posterior blepharitis affects the inner part of the eyelid margins and openings of the meibomian glands, glands along the inner rim of the eyelids that produce oil
Both anterior and posterior blepharitis may be present at the same time.
What causes blepharitis?
Blepharitis can be caused by bacteria (staphylococcal blepharitis) or dandruff on the skin (seborrheic blepharitis). Blepharitis can also be caused by allergies or small mites that live on the skin and eyelashes, called Demodex [6].
The most common cause of posterior blepharitis is a condition called meibomian gland dysfunction, where the meibomian glands either do not produce enough oil, or produce oils that are of very poor quality [7]. There are a number of factors that can affect meibomian gland secretions, including ageing, hormone changes, trauma, reduced blinking, and certain medications [8].
How does blepharitis develop?
When there is an overload of bacteria or dandruff on the skin near the eyes, the eyelids can become irritated and inflamed. The inflammation can also be due a reaction to allergens or other irritants on the skin.
If there are Demodex mites present on the skin, the toxins and shedding from the mites can also cause skin irritation and blepharitis.
What conditions are associated with blepharitis?
Blepharitis is more common in people with inflammatory skin conditions, such as eczema (atopic dermatitis) and acne rosacea. People with blepharitis can also develop inflammation in other parts of the eye. A common condition is conjunctivitis, which is an inflammation of the transparent tissue that covers the white parts of the eye.
Posterior blepharitis is associated with dry eye disease. The oils produced by meibomian glands form an important part of the tear film that stops tears from evaporating. When the oil production is affected, the tears evaporate faster.
What are the common signs and symptoms of blepharitis?
Some of the common signs and symptoms of blepharitis include the following:
- Burning or stinging sensation in the eye
- Itchiness along the eyelid margins
- Sticky eyelids or crusty eyelids or eyelashes when you wake up
- Gritty sensation or feeling like there is something in the eye
- Red and swollen eyelids or eyes
- Watery eyes
- Vision that fluctuates when you blink
- Dry eyes that make you feel like you need to blink a lot
- Tears that are foamy or have small bubbles in them
- Mild sensitivity to light
- In some cases, eyelashes that become misdirected or fall out
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
Different severities of blepharitis
Some people with blepharitis do not have any symptoms, and some people only experience mild irritation and discomfort. Generally, the more inflamed that a person’s eyelids are, the more frequent and severe their symptoms might be. However, this is not always the case.
In some cases, blepharitis that is not treated can lead to other diseases, such as:
- Loss of eyelashes
- Thickening of eyelid margins
- Hordeolum, a red lump that is tender or painful, caused by the infection of a blocked oil gland on the eyelid
- Chalazion, a painless, firm lump caused by prolonged inflammation of the oil gland of the eyelid
- Infection of the other tissues in the front of the eye, such as the cornea, the clear and transparent part of the eye. If left untreated, corneal infections can cause damage to vision
How is blepharitis diagnosed?
Blepharitis is usually diagnosed by an eye health professional during a comprehensive eye examination. This includes finding out about any symptoms (such as itching or grittiness), performing a vision test, and a detailed assessment of the front of the eyes.
Some people have blepharitis but do not know it, or they experience symptoms of blepharitis, but have not been told that blepharitis is the cause. This is why it is important to follow the recommendations for how regularly a person should have an eye check.
How does an eye health professional confirm that you have blepharitis?
The eye health professional will closely examine the front of the eyes, eyelids, and eyelashes. This is usually performed using a biomicroscope, which is an instrument that shines an external light onto the eyes and allows the examiner to look at different eye structures under magnification.
The eye health professional may gently squeeze your eyelid margins to look at the colour, thickness, and texture of the oils that are released from your meibomian glands. They may also put in some ocular dyes (such as sodium fluorescein, which is a non-toxic yellow dye) in the eyes to assess your tear film and to see if there are any damaged cells in the front of the eyes.
Sometimes, the eye health professional will use an imaging device with specialised illumination to assess the quality of your tears and the health of your meibomian glands.

How is blepharitis treated?
The main goals for treating blepharitis are to treat the cause of the inflammation and to alleviate its symptoms. Some of the treatment options for blepharitis include the following:
Lid hygiene
For treating anterior blepharitis, the eyelids should be cleaned regularly to wash off any dandruff, bacteria, and build-up of debris around the eyelash base. This can be done by using over-the-counter lid cleaning products applied to the lash margins with a swab or cotton bud. If a dedicated eyelid cleaner is not available, a mixture of water and baby shampoo can also be used [9]. Just like dandruff in other parts of the body, cleaning the eyelids regularly is needed to prevent a build-up.
Warm compresses
If the meibomian glands are not healthy or are not producing oils, warm compresses can improve the amount and quality of oils that are produced from these glands. This can be done by heating up the glands with a warm (35-45 °C) heat pack for 5-10 minutes, then gently massaging the eyelids to help express the oils from the glands. This routine should be repeated regularly to restore oil flow from the meibomian glands.
Other treatments
Antibiotics
A specific type of oral antibiotic medications that have anti-inflammatory effects may be prescribed to help reduce the inflammation around the eyelids. A topical antibiotic eye drop or cream may be prescribed to reduce the bacterial load on the eyelids.
Lubricating eye drops
Symptoms of grittiness and dryness can be improved with lubricating eye drops, or artificial tear supplements. These eye drops contain substances that replace tears that are lost to evaporation, to improve symptoms.
Tea tree oil
If a person has blepharitis caused by Demodex mites, cleaning the lids with a solution of diluted tea tree oil can help reduce the number of mites on the eyelids [6].
Dietary interventions
Increasing dietary intake of foods that have anti-inflammatory properties, such as oily fish that contain omega-3 fatty acids, can also reduce symptoms associated with blepharitis [10, 11].
In-clinic treatments
Other treatments that may be performed by an eye health professional in the clinic include using eyelid-warming devices to heat the meibomian glands [11], manually expressing the meibomian glands, and using light to stimulate oil flow from the glands in the eyelids [12].
Can I prevent blepharitis?
Blepharitis can be prevented by keeping the eyelids clean. This can reduce the build-up of bacteria and dandruff on the eyelids and eyelashes.
When using eye make-up, care can be taken to reduce the build-up of bacteria on the eyelids by using non-oil-based eye make-up products, cleaning make-up brushes often, not using expired products, and cleaning the eyelids carefully.
Poor compliance to treatment is a major reason why blepharitis can reoccur. Studies have shown that only half of the people who start treatments to keep their lids clean continue to do so after six weeks [13]. It is important that the treatment that is recommended by an eye health professional is maintained to prevent blepharitis from reoccurring.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- M. A. Lemp and K. K. Nichols, “Blepharitis in the United States 2009: A Survey-based Perspective on Prevalence and Treatment,” Ocul Surf, vol. 7, no. 2, Supplement, pp. S1-S14, 2009/04/01/ 2009, doi: https://doi.org/10.1016/S1542-0124(12)70620-1.
- D. F. Rabensteiner, H. Aminfar, I. Boldin, G. Schwantzer, and J. Horwath-Winter, “The prevalence of meibomian gland dysfunction, tear film and ocular surface parameters in an Austrian dry eye clinic population,” (in eng), Acta ophthalmologica, vol. 96, no. 6, pp. e707-e711, 2018, doi: 10.1111/aos.13732.
- “The epidemiology of dry eye disease: report of the Epidemiology Subcommittee of the International Dry Eye WorkShop (2007),” (in eng), Ocul Surf, vol. 5, no. 2, pp. 93-107, Apr 2007, doi: 10.1016/s1542-0124(12)70082-4.
- T. H. Rim, M. J. Kang, M. Choi, K. Y. Seo, and S. S. Kim, “Ten-year incidence and prevalence of clinically diagnosed blepharitis in South Korea: a nationwide population-based cohort study,” Clinical & Experimental Ophthalmology, vol. 45, no. 5, pp. 448-454, 2017, doi: https://doi.org/10.1111/ceo.12929.
- N. Gupta, A. Dhawan, S. Beri, and P. D’Souza, “Clinical spectrum of pediatric blepharokeratoconjunctivitis,” (in eng), J aapos, vol. 14, no. 6, pp. 527-9, Dec 2010, doi: 10.1016/j.jaapos.2010.09.013.
- A. C. Zhang, A. Muntz, M. T. M. Wang, J. P. Craig, and L. E. Downie, “Ocular Demodex: a systematic review of the clinical literature,” Ophthalmic Physiol Opt, vol. 40, no. 4, pp. 389-432, 2020/07/01 2020, doi: 10.1111/opo.12691.
- K. K. Nichols et al., “The International Workshop on Meibomian Gland Dysfunction: Executive Summary,” Investigative Ophthalmology & Visual Science, vol. 52, no. 4, pp. 1922-1929, 2011, doi: 10.1167/iovs.10-6997a.
- C. Baudouin et al., “Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction,” Br J Ophthalmol, vol. 100, no. 3, pp. 300-306, 2016, doi: 10.1136/bjophthalmol-2015-307415.
- J. Sung et al., “Randomized double-masked trial of eyelid cleansing treatments for blepharitis,” (in eng), Ocul Surf, vol. 16, no. 1, pp. 77-83, Jan 2018, doi: 10.1016/j.jtos.2017.10.005.
- A. C. Zhang, S. Singh, J. P. Craig, and L. E. Downie, “Omega-3 Fatty Acids and Eye Health: Opinions and Self-Reported Practice Behaviors of Optometrists in Australia and New Zealand,” (in eng), Nutrients, vol. 12, no. 4, p. 1179, 2020, doi: 10.3390/nu12041179.
- L. Jones et al., “TFOS DEWS II Management and Therapy Report,” (in eng), Ocul Surf, vol. 15, no. 3, pp. 575-628, Jul 2017, doi: 10.1016/j.jtos.2017.05.006.
- S. Cote et al., “Intense pulsed light (IPL) therapy for the treatment of meibomian gland dysfunction,” Cochrane Database of Systematic Reviews, no. 3, 2020, doi: 10.1002/14651858.CD013559.
- Y. A. Alghamdi, A. Camp, W. Feuer, C. L. Karp, S. Wellik, and A. Galor, “Compliance and Subjective Patient Responses to Eyelid Hygiene,” (in eng), Eye Contact Lens, vol. 43, no. 4, pp. 213-217, Jul 2017, doi: 10.1097/icl.0000000000000258.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
