Macular Dystrophies
Macular dystrophies – Written by Associate Professor Lauren Ayton, B Optom, PhD, FAAO, FACO.
What are macular dystrophies?
Macular dystrophies are a group of rare inherited diseases which affect the central region of the retina, known as the macula. This region of the eye is responsible for central and colour vision, so damage to the macula causes deterioration of these aspects of sight.
Sometimes people confuse macular dystrophies, which are rare, with the more common age-related macular degeneration. Both of these conditions cause progressive damage to the macula, and central vision loss. However, there are some main differences, as shown in Table 1.
Table 1: Differences between macular dystrophies and age-related macular degeneration
| Macular dystrophies | Age-related macular degeneration | |
| Cause | Mainly genetic | Some genetic factors, but also linked to environmental risks such as smoking |
| Age of onset | Earlier in life (can be in childhood) | Over the age of 55 years |
| Clinical presentation | Usually, symmetrical | Common to be worse in one eye than the other |
This overview will cover the different types of macular dystrophy, its common signs and symptoms, the ways that it is diagnosed, as well as what the future holds for people with the disease.
What are the types of macular dystrophy?
There are a number of different subtypes of macular dystrophy, which are caused by different genetic mutations. The most common of these are Stargardt’s Disease, which accounts for around 7% of all cases of macular dystrophy [1], and Best Disease. There are also other rarer forms of the disease.
Stargardt’s Disease
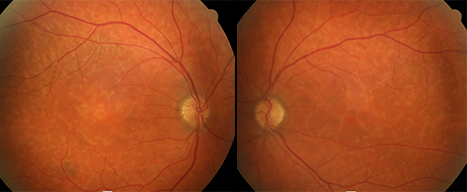
This is the most common form of macular dystrophy, and is normally detected in childhood. Stargardt’s affects 1 in 10,000 people worldwide. It is caused by a mutation in the ABCA4 gene [2]. There is a variation of Stargardt’s, called fundus flavimaculatus, which affects older individuals, and is usually milder [3]. Clinically, Stargardt’s disease is identified by flecks at the macula which are elongated and are often said to look like fish tails [3]. (Figure 1).
Best Disease
Also known as vitelliform macular dystrophy, Best disease has a characteristic clinical appearance. Due to the accumulation of a fatty yellow pigment (called lipofuscin), a central yellow lesion that looks like an egg yolk forms at the macula (Figure 2) [4]. Best disease usually starts in childhood, but an adult-onset version also exists. It is due to mutations in various genes, including BEST1. It has a similar prevalence to Stargardt’s disease, occurring in approximately 1 in 10,000 people [4].

Genetic testing for macular dystrophies
To confirm if a person has macular dystrophy and, if they do, what subtype, genetic testing will often be recommended. Genetic testing can be accessed through ophthalmologists and clinical genetics services (both public and private). It is also important to undertake genetic counselling, which will provide explanation of the results, and what they mean for an individual. This is particularly important for people who are family planning.
What are the common signs and symptoms of macular dystrophies?
Macular dystrophies all cause damage to the central region of the retina (macula). Hence, symptoms include loss of vision and blurriness in the centre of the visual field. This can make tasks like reading and face recognition difficult. Usually, people with the condition maintain their peripheral (side) vision. Macular dystrophies also cause loss of colour vision.
Sometimes people with the disease find that they are more sensitive to light, and need more time to adjust between light and dark environments. Dark tinted sunglasses can help make vision more comfortable in some settings.
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How are macular dystrophies diagnosed?
Macular dystrophies are diagnosed by an ophthalmologist through a range of eye tests. Many of these tests are standard clinical care, including measurement of vision, assessment of the back of the eye and retina, and taking photos and scans of the eye. The retina shows characteristic changes at the macula, including white and yellow deposits, and areas of cell loss (atrophy).
Specialised tests are often needed to confirm the diagnosis of macular dystrophy. One example is an electroretinogram, which is a test that records the electrical activity of the retina in response to light. It is similar to an electrocardiogram (ECG) test and requires specialised equipment and technicians.
Another common clinical test for macular dystrophies is an optical coherence tomography (OCT) image, which takes a cross-sectional scan of the retina so that the eyecare practitioner can assess which cell types have been damaged. This is a quick, painless test, similar to having a photograph taken.
Often diagnosis of macular dystrophy requires referral to a specialist ophthalmologist, who is an expert in inherited retinal diseases.
How are macular dystrophies treated?
At the moment, there are no specific treatments for macular dystrophies.
Can I reduce the risk of developing macular dystrophies?
As macular dystrophies are caused by genetics, it is not possible to reduce the risk of developing the conditions.
What does the future hold for people with macular dystrophies?
A number of experimental treatments for macular dystrophies are currently in development, including gene therapy and stem cells. Studies are also underway into drugs that can improve metabolism of Vitamin A and help clear toxic waste products from the retina.
There are a number of excellent support services available for people with macular dystrophies. These include training in low vision aids, such as magnifiers, electronic reading equipment and smartphone technology, which can make life easier with central vision loss.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- Strauss RW, Munoz B, Ahmed MI, et al. The Progression of the Stargardt Disease Type 4 (ProgStar-4) Study: Design and Baseline Characteristics (ProgStar-4 Report No. 1). Ophthalmic Res 2018;60(3):185-94.
- Bok D. Cellular mechanisms of retinal degenerations: RPE65, ABCA4, RDS, and bicarbonate transporter genes as examples. Retina 2005;25(8 Suppl):S18-S20.
- Hadden OB, Gass JD. Fundus flavimaculatus and Stargardt’s disease. Am J Ophthalmol 1976;82(4):527-39.
- Stone EM, Nichols BE, Streb LM, et al. Genetic linkage of vitelliform macular degeneration (Best’s disease) to chromosome 11q13. Nat Genet 1992;1(4):246-50.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
