Cataract
Cataract – Written by Purrven Bajjaj, B Optom, MSc Clinical Optom.
What is a cataract?
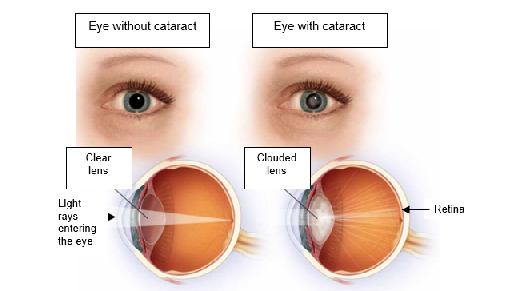
A cataract occurs when an opaque or cloudy area develops in the normally clear lens (responsible for the focusing mechanism) of the eye. This cloudy area scatters and blocks the light as it passes through the lens, preventing a clear image from reaching the retina (light-sensitive tissue at the back of the eye). Clouded vision caused by cataracts is often described as seeing through a frosty or foggy window. When the cloudy vision interferes with daily activities such as reading or driving a car, undergoing surgery is recommended to remove the cataract.
The following sections will briefly outline the global problem and economic impact of cataract, how it forms, its various types, its risk factors, its signs and symptoms, and some insights into its treatment options.
The global problem of cataract
Globally, is the leading cause of blindness and the second cause of partial vision loss. A large study conducted in 21 countries reported that in 2020, cataract was the leading cause of blindness in those aged 50 years and older [1].
Global estimates show that approximately 2.2 billion people suffer from total or partial vision loss, out of which, about 65 million is due to cataract. According to the National Eye Institute in the United States (US), the number of people with the condition in the US is expected to double from 24.4 million to about 50 million by the year 2050 [2].
The economic impact of cataract
Cataract is known to cause blindness or partial vision loss, potentially affecting an individual’s ability to work. Surgery is available to treat and remove cataracts to prevent blindness or partial vision loss. Barriers in low-income countries such as the lack of health insurance, inability to afford surgery, or lack of suitable eye health facilities hinders the treatment of cataracts through surgery.
Researchers have found that people who have undergone cataract surgery are able to increase their economic productivity by approximately 15 times the cost of the surgery during the first year after surgery [3]. A study done at a large chain hospital in India, the Aravind Eye Hospital, reported that about 6 in 10 women who lost their jobs as a result of becoming blind due to cataract regained their jobs after cataract-removal surgery [4].
How does a cataract form?
Cataracts form when proteins in the lens of the eye clump together, making the lens cloudy. The lens of the eye is normally clear, allowing light to pass through. The lens allows the focusing of light on the retina (light sensitive tissue at the back of the eye) to produce clear vision, and mostly consists of water and proteins.
In an eye without cataract, the proteins line up in a manner such that it enables the lens to be completely clear, allowing light to pass through easily. If proteins in the lens clump together, the lens gets cloudy and light cannot pass through the clumps of protein in the lens easily, resulting in decreased vision. Over time, as the clumps of protein become larger and thicker, vision is further decreased.
Types of cataracts
The following section covers the various types of cataracts.
Nuclear cataract
A nuclear cataract refers to the hardening of the nucleus or center of the lens of the eye. Nuclear cataract may cause an increase in the onset of myopia (short-sightedness). In the initial stages of nuclear cataract, the lens becomes cloudy and yellow. As the condition progresses, the lens may turn brown and harden. People with nuclear cataract may have difficulty distinguishing between shades of colour due to yellowing or browning of the lens.

Cortical cataract
In cortical cataract, areas of white cloudiness develop in the outer edges of the lens called the cortex. These areas of cloudiness spread inward and appear like spoke wheels or in a star pattern. People with cortical cataract experience blurred vision and glare as light entering the eye is scattered and a decrease in contrast is observed as well.

Posterior subcapsular cataract
Posterior subcapsular cataract (PSSC) begins as a cloudy or opaque area on the back surface or posterior of the lens. PSSC develops below the lens capsule, hence the name ‘subcapsular’. The lens capsule is a sac-like membrane that holds the lens in place. When PSSC begins to develop, it usually does so rapidly and symptoms such as glare, presence of haloes around light, and difficulty reading are noticed a few months after PSSC begins to develop.

Cataracts in children
Children can get cataracts too and they may be present at birth (congenital cataracts) or develop as they grow (paediatric cataract).
Congenital cataract is the clouding of the lens of the eye that is present at birth. Clouding of the lens causes blurring of vision as light cannot reach the retina (light-sensitive tissue at the back of the eye). Without early intervention, this can affect children’s visual development, causing other sight-threatening conditions such as lazy eye, nystagmus, inability to fix and focus on objects, and even blindness.
If the cataract only affects a small part of the lens and does not interfere with vision, surgery is not required. However, if the cataract is dense and affects vision, congenital cataracts may need to be removed during infancy.
Among children with congenital cataracts, 1 in 4 cases is attributed to genetics [5], which means that they probably inherited the genes from either parent. Other congenital cataracts may occur due to trauma, diabetes, myotonic dystrophy, galactosemia, neurofibromatosis or rubella. To detect congenital cataracts, it is important to ensure that children undergo routine eye checkups.
Children may also develop another type of cataract known as paediatric cataract, which may also occur due to trauma, diabetes, or may be inherited from either parent. Trauma directly to the eye accounts for 40% of the paediatric cataract cases [6].
Traumatic cataract
Traumatic cataract is clouding of the lens that may occur after a blunt trauma (when an object collides with the eye but does not cut the eye or face with force) or sharp trauma (when an object collides with the eye and face with force, hitting the eye and disrupting the lens fibers). It is essential to avoid eye injuries and trauma as much as possible by taking appropriate measures like using protective eyewear such as glasses and eye shields when dealing with potentially hazardous situations.
Radiation cataract
The lens is the most radiosensitive structure of the eye. Radiation cataract is clouding of the lens resulting from damaged cells, covering the posterior (back) surface of the lens. Cell damage occurs due to over exposure to radiation. Ultraviolet rays from the sun and radiation treatment for cancer can cause radiation cataracts. Blurring of vision from radiation cataracts may occur 1 or 2 years following high radiation exposure and many years after exposure to low radiation doses [7].
Risk factors for cataract
Cataracts can be present at birth or may develop as a natural part of the ageing process. Age-related cataracts (nuclear cataracts, cortical cataracts and posterior subcapsular cataract) are known to develop faster and risk factors contributing to these types of cataracts are mentioned below.
Smoking
Studies have found that smokers are twice as likely to develop cataracts as compared to those who do not smoke [8].
Diabetes
Studies indicate that cataract is about 4 times more common among people under the age of 65 who have diabetes [9]. For people over the age of 65 with diabetes, cataracts are twice as prevalent than those with no diabetes [10]. The longer the duration of someone suffering from diabetes and the poorer the control of their diabetes, the higher the risk of developing cataract.
Medications
Taking high doses of steroids for prolonged periods can cause posterior subcapsular cataracts to form.
Spending too much time under the sun
According to the World Health Organization, 1 out of 5 cataracts could be prevented with proper eye protection or reduced exposure to direct sunlight.
Radiation treatment
Radiation treatment for cancer or other diseases can result in an earlier onset of cataract. Symptoms can either appear as early as 1 to 2 years following high doses of exposure or many years after exposure to lower doses.
Complications from cataract
Cataracts are not usually dangerous to eye health until they become completely white, referred to as overripe or hypermature cataract. This can cause an increase in eye pressure and present suddenly with redness, pain in the eye, and/or headaches, and will need to be removed.
What are some of the common signs and symptoms of cataract?
When cataract initially develops, it may only affect a small part of the lens and symptoms may not be present or mild, if any. As the condition progresses, it clouds more of the lens and scatters the light passing through the lens, making symptoms more noticeable.

- Blurry or cloudy vision that cannot be corrected with glasses or contact lenses
- Increasing difficulty with vision at night
- Need for brighter light when reading and engaging in other activities
- Glare
- Presence of haloes around light sources
- Fading of colours, sometimes with a yellowish tint
- Double vision in one eye
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is cataract diagnosed?
Cataract is diagnosed by trained eye health professionals through a comprehensive eye health check. To allow for better and wider examination of the eye, drops are often used to dilate or widen the pupil (dark spot in the centre of the eye) and the eye health professional will then do a dilated eye exam. Dilation drops take about 30 minutes to effectively dilate the pupil for examination and will cause a temporary blurring of vision that resolves after about 4 to 6 hours.
After assessing the health of the eye, the eye health professional will then grade the cataract by following a grading scale which categorises the types of cataracts according to their severity. Grading scales differ between countries. When the cataract is deemed to be severe or causing a significant decrease in vision and ability to perform daily activities, the eye health professional will then recommend surgery.
How is a cataract treated?

Cataract surgery
Surgery is the only known treatment for cataract. It is where the surgeon removes the clouded lens and replaces it with a new, artificial lens, also known as an intraocular lens (IOL) that becomes a permanent part of the eye. Cataract surgery is performed as a day surgery and is usually performed with topical instead of general anaesthesia.
Cataract surgery is known to improve the quality of life of patients by approximately 40% when performed in both eyes [11]. 9 in 10 people report better vision after undergoing surgery to remove cataracts [12].
Cataract surgery process
1. Phacoemulsification cataract surgery
Most cataract surgeries are performed with a technique referred to as phacoemulsification, which removes the need for stiches. The procedure involves making a small incision on the cornea (transparent jelly like layer protecting the front of the eye). An instrument that vibrates is then introduced in the eye via this incision in a process called emulsification or softening of the lens.
The clouded lens is then sucked out through the instrument and the capsule of the lens remains to receive the artificial lens implant or IOL. There are various types of IOLs available and after discussing your needs and expected visual outcome after surgery, the eye health professional will recommend the most suitable option accordingly.
2. Femtosecond laser-assisted cataract surgery
A more recently established technique for cataract removal, is femtosecond laser-assisted cataract surgery (FLACS), which involves a process very similar to that of PCS, but the surgeon uses a femtosecond laser instead of ultrasound waves to breakdown the cataract.
This method of cataract eye surgery is considered by some ophthalmologists to be a better option, as it allows for a more precise surgery, and limits the amount of damage that ultrasound waves can potentially cause to surrounding tissues. However, a study published in The Lancet Journal found that FLACS did not provide any added benefits for patients when compared to PCS.
Post-cataract surgery healing
After surgery, your doctor might recommend that you wear an eye patch or eye guard to protect your eye in the first few days of its healing, and you might be given eye drops to administer to prevent infection. Your vision may be blurry at first, and it is normal to experience mild itching and discomfort after the operation. It is especially important during the first few weeks of recovery that you avoid rubbing or pressing on your eye. Healing from this operation normally takes around 8 weeks. When your clear vision is returning colours might appear brighter than usual with your new clear lens.
Cataract surgery risks
As with many medical procedures, there are some risks involved in cataract surgery. However, complications are uncommon and often easy to treat in the case of cataract surgery. The most common complications include:
- Inflammation
- Infection
- Drooping eyelid
But in extremely rare cases, some people experience retinal detachment, a condition that is considered a medical emergency, where the retina becomes detached and threatens permanent sight loss. Another rare complication of cataract surgery is a secondary cataract.
Tips to manage cataract
In the initial stages, before surgery is recommended, the following are some tips that can be useful for people with cataract:
- Use sunglasses and if possible, accompanied with a wide brim hat when spending time outdoors to protect the eyes from UV rays
- Increase the lighting when reading or engaging in other activities
- Cataracts can cause changes in the prescription of our eyes. A new prescription for glasses or contact lenses can improve vision with cataracts, early on.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- “Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study”, The Lancet Global Health, vol. 9, no. 2, pp. 144-160, Dec 2020, doi: https://doi.org/10.1016/S2214-109X(20)30489-7
- “Cataract data and statistics”, National Eye Institute. [Online]. Available: https://www.nei.nih.gov/learn-about-eye-health/outreach-campaigns-and-resources/eye-health-data-and-statistics/cataract-data-and-statistics. [Accessed: 19 Aug 2021]
- Y. C. Liu et al., “Cataracts”, The Lancet, vol. 390, no. 10094, pp. 600-12, Aug 2017, doi: https://doi.org/10.1016/S0140-6736(17)30544-5
- D. T. Jamison et al., “Impact of cataract surgery on individuals in India”, Disease Control Priorities in Developing Countries, New York, Oxford University Press for the World Bank: 1993. [Accessed 03 Jan 2011]
- Merin S. “Inherited Cataracts”, Inherited Eye Diseases. Marcel Dekker Inc: New York: 1991. Pp. 86-120
- Y. N. Xu, Y. S. Huang and L. X. Xie, “Pediatric traumatic cataract and suagery outcomes in eastern China: a hospital-based study”, Int J Ophthalmol, vol. 6, no. 2, pp. 160-164, Apr 2013, doi: 10.3980/j.issn.2222-3959.2013.02.10
- “Radiation Cataract (Lens Opacity), Radiation Effects Research Foundation. [Online]. Available:https://www.rerf.or.jp/en/programs/roadmap_e/health_effects-en/early-en/cataract_en/#:~:text=Radiation%20cataract%20causes%20partial%20opacity,after%20exposure%20to%20lower%20doses. [Accessed: 19 Aug 2021]
- “Cataracts”,Brobergeyecare.[Online].Available: https://brobergeyecare.com/cataracts/smoking-and-the-increased-risk-of-cataracts/#:~:text=Cataracts%20should%20be%20a%20real,the%20greater%20that%20risk%20becomes. [Accessed: 19 Aug 2021]
- B. E. Klein, R. Klein and S. E. Moss, “Prevalence of cataracts in a population-based study of persons with diabetes melitus”, Ophthalmology, vol. 92, no. 9, pp. 1191-6, Sep 1985.
- F. Ederer, R. Hiller and H. R. Taylor, “Senile lens changes and diabetes in two population studies”, Am J Ophthalmol, vol. 91, no. 3, pp. 381-95, Mar 1981.
- G. Brown et al., “The Extraordinary Patient Value and Financial Value to Society Conferred by Cataract Surgery”, Ophthalmology, pp. 2367-76, Dec 2013.
- “Cataract”.[Online].Available:https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/cataract?sso=y. [Accessed: 19 Aug 2021]
- H Hashemi et al,. “Global and regional prevalence of age-related cataract: a comprehensive systematic review and meta-analysis.”, Eye vol. 34, pp. 1357–70, Feb 2020, doi: https://doi.org/10.1038/s41433-020-0806-3
- A. Foster., “Vision 2020: The cataract challenge”, Community Eye Health, vol. 13, no. 34, pp. 17-19, 2000.
- M. Z. Wale et al., “Cataract and associated factors among adults visiting ophthalmic clinic at Debre Markos comprehensive specialized hospital, northwest Ethiopia, 2020”, vol. 9, Jan 2021, doi: https://doi.org/10.1177/2050312121989636
- Tej Kohli., “To end extreme poverty, we must also end blindness”, June 2021. [Online]. Available: https://www.weforum.org/agenda/2021/06/to-end-extreme-poverty-we-must-also-end-blindness/. [Accessed: 19 Aug 2021]
- “Blindness and vision impairment”, Feb 2021. [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. [Accessed: 19 Aug 2021]
- C. Fong et al., “Correction of Visual Impairment by Catract Surgery and Improved Survival in Older Persons”, Ophthalmology, pp. 1720-27, Sep 2013
- J. W. Y. Yau et al., “Global prevalence and major risk factors of diabetic retinopathy”, Diabetes Care, vol. 35, no. 3, pp. 556-64, Mar 2021, doi: 10.2337/dc11-1909
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
