Chalazion and stye
Chalazion and stye – Written by Dr. Vivian Kuang, MBBS (Hons) and Dr. Elsie Chan, B.Sc(Med) Hons, MBBS(Hons), MPH, FRANZCO.
What is a chalazion and a stye?
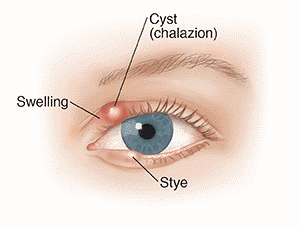
Chalazia (plural of chalazion, also known as meibomian cysts) and styes (also known as a hordeolum) are common types of inflammatory lumps that form inside or on the edge of the upper or lower eyelids. They can affect one or both eyes and there can be more than one lump at a time. They are benign (non-cancerous) and are not usually vision threatening but may be troublesome when they are large or recurring, or if they become infected. While the terms chalazion and stye are often used interchangeably for eyelid lumps, they are in fact, different.
The following sections will briefly outline the difference between a chalazion and stye, what causes them to develop, their signs and symptoms, and some insights into their treatment.
What is the difference between a chalazion and a stye?
A chalazion is a lump on the eyelid caused by the blockage of an oil gland (called a meibomian gland). It is generally not tender unless there is associated inflammation.

A stye is a small, red, painful lump at the eyelid margin which is caused by an infected gland (usually a Staphylococcal infection). There are two types of styes, known as internal or external hordeola (plural of hordeolum).
- An internal hordeolum is a stye that forms from a meibomian gland and appears as a red lump inside the eyelid.
- An external hordeolum is a stye that forms at the base of an eyelash (from glands called ‘glands of Zeiss’ or ‘glands of Moll’) and has the appearance of a pimple of the outer edge of the eyelid.

Sometimes, it is difficult to tell the difference between a chalazion and a stye, especially internal hordeolum and chalazion. However, styes are typically red, painful and cause more swelling of the eyelid than a chalazion. Chalazion and internal hordeolum form deeper in the eyelid than external hordeolum.
How common is a chalazion and a stye?
Chalazion and styes are one of the most common types of eyelid lumps worldwide. While they affect people of all ages, they are more commonly seen in children and adults under 30 years old. The exact incidence is difficult to determine as many people with these lumps do not seek medical attention but is reported to range between 0.2 to 0.7% [2]. They affect people of all races with no difference between males and females [3]. They are more common in the upper lid, due to the increased number of glands in the upper lids compared to lower lids.
What causes a chalazion and a stye?
A chalazion is usually caused by a non-infected blockage of the meibomian (oil) gland.
A stye is usually caused by infection with bacteria called Staphylococcus aureus [1]. Staphylococcus bacteria normally reside on the skin but may cause infection if the skin is broken or damaged.
Chalazion or styes are more likely to form in people who have:
- Had one before
- Eyelid conditions such as blepharitis (inflammation of the eyelids)
- Skin conditions such as eczema, acne rosacea or seborrheic dermatitis
- Exposure to air pollutants which block the meibomian glands [2], [3]
What are their common signs and symptoms?
The common signs and symptoms of a chalazion include:
- Firm ‘pea-like’ lump with or without mild redness and/or swelling of the eyelid
- Blurry vision if a large chalazion presses on the front surface of the eye
- Drooping of the eyelid if the chalazion is large
The common signs and symptoms of a stye include:
- Small, red, painful lump on the eyelid margin with or without eyelid swelling
- Feeling as if something is stuck in the eye
- Crusting of the eyelids or lashes
- A white or yellow ‘top’ from where the infection may spontaneously drain
- Discharge – if it is expressed from the infected gland
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is a chalazion and a stye diagnosed?
An eye health professional can diagnose a chalazion or stye by examining the external surface and underside of the eyelids. The eye health professional may also use a special microscope known as a slit lamp. Further tests are usually not required. However, if the appearance is not typical for a chalazion or stye, a biopsy (where a small sample of tissue is taken under local anaesthetic) may be required.
What treatment options are there?
In most cases, a chalazion or stye resolves on its own over weeks to months without any treatment or surgery [4].
Warm compresses
The recommended treatment for a chalazion and stye is warm compress (holding a clean towel or washcloth which has been soaked in hot water against the eyelids, or using a heat pack) followed by gentle massage of the lump for 10-15 minutes, several times per day. The eyelids should be kept clean with lid scrubs using a saline solution or baby shampoo diluted in warm water. To allow healing and prevent aggravation, eye makeup and contact lenses should be avoided.

Antibiotics
Antibiotic eye drops or tablets are not usually required. However, antibiotic tablets may be recommended if there is an infection of the surrounding eyelid skin, or to treat severe blepharitis (inflammation of the eyelid margin).
Surgical treatments
If a chalazion persists (for about 1 month or longer), surgical management is generally considered. It involves surgery to drain the lump under local anaesthetic. Less commonly, an injection of steroid medication into the lesion may help (if there is no infection). Drainage should not be performed without an eye health practitioner as it can lead to scarring and infection.
A chalazion or stye that does not resolve or recur in the same location require referral to an ophthalmologist (an eye doctor with medical training), to exclude other potentially serious causes for eyelid lumps.
What are the possible complications from a chalazion and a stye?
In severe cases, a chalazion and styes can lead to infection of the eyelid and surrounding soft tissue (pre-septal cellulitis) requiring treatment with oral antibiotics, an antibiotic injection into a muscle in the arm, or through an intravenous drip.
When a chalazion gets very large, it can cause blurry vision due to pressure on the cornea (the clear window at the front of the eye). This causes the cornea to change shape, altering the eye’s ability to focus. This is of particular concern in young children (younger than 8 years old) as their vision is still developing at this age.
How can I prevent a chalazion and a stye from forming?
A chalazion or stye may be prevented by treating the risk factors that lead to their development. If there is an underlying eyelid or general health problem that is contributing, this should be managed with the relevant health care practitioner.
Good eyelid hygiene is essential, including:
- Washing hands regularly and avoid touching the eyes and eyelids with hands or dirty towels
- Thoroughly washing off eye makeup and replacing products at recommended schedules
- Regular lid cleaning with warm compresses and eyelid scrub.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- B. Mueller and C. M. McStay, “Ocular infection and inflammation,” Emerg Med Clin North Am, vol. 26, no. 1, pp. 57-72, Feb 2008, doi:10.1016/j.emc.2007.10.004
- Alsammahi et al., “Incidence and predisposing factors to chalazion,” Int J Community Med Public Health, vol. 5, no. 11, pp. 4979-4982, Nov 2018, doi:http://dx.doi.org/10.18203/2394-6040.ijcmph20184253
- Y. Nemet, S. Vinker and I. Kaiserman, “Associated morbidity of chalazia,” Cornea, vol. 30, no. 12, pp. 1376-1381, Dec 2011, doi:10.1097/ICO.0b013e31821de36f
- Kindsley, J. J. Nichols and K. Dickersin, “Interventions for acute internal hordeolum,” Cochrane Database Syst Rev, vol. 2010, no. 9, pp. CD007742, Sep 2010, doi: 10.1002/14651858.CD007742.pub2
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
