Colour Blindness and Colour Vision Deficiencies
Colour blindness and colour vision deficiencies – Written by Dr. Amanda Douglass, B Optom, GCUT, Ph.D., FHEA.
What is colour vision deficiency?
Colour vision deficiency, often referred to as “colour blindness”, refers to the collection of disorders that cause the inability to discriminate between different colours. This can result in difficulty discriminating similar colours (difficulty with different shades), or difficulty discriminating dissimilar colours (for example red and green). In rare cases, there is a complete inability to distinguish colour, instead differentiating objects based only on their brightness.
The following sections will first explain how our eyes see colour, and then outline how common colour vision deficiencies are, what causes colour vision deficiency, its signs and symptoms, and some insights into its management and treatment.
How do we see colour?
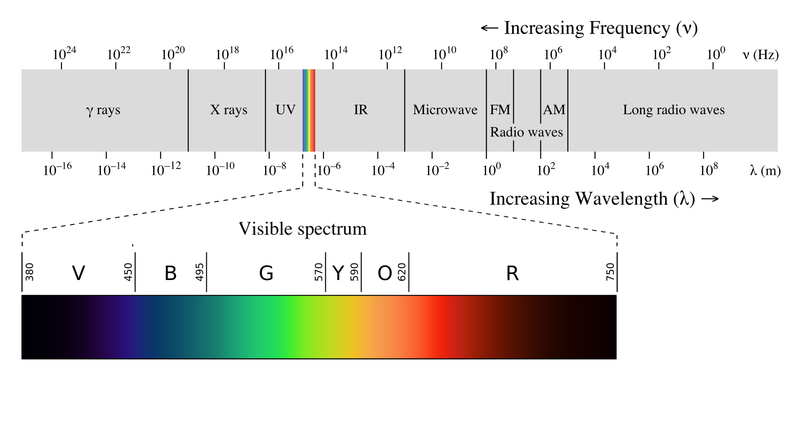
Light is the part of the electromagnetic spectrum that our eye is able to respond to; it is the part we can “see” (Figure 1). Within the eye there are cells which respond to light: rods and cones. Our response to light from different parts of the spectrum creates the experience of colour.
Colour vision begins with the cones in our eyes. There are three cone types containing pigments with different sensitivities to the parts of visible light spectrum [1] (Figure 2). The three different cone types are:
- Long-wavelength sensitive (red cones),
- Medium-wavelength sensitive (green cones)
- Short wavelength sensitive (blue cones).

Light is absorbed by the pigment which triggers a response from the cone. Each cone does not differentiate colour, it simply responds based on its sensitivity to the wavelengths the light is made up of. The cones then send their response along the visual pathway via separate colour channels to the brain: red versus green and blue vs yellow (yellow created by red and green cones combined) [2]. The brain then interprets the relative responses from the three different cones to create colour perception [3] (Figure 3).

How common are colour vision deficiencies?
Congenital colour vision deficiency (present from birth) affects approximately 8% of males and 0.4% of females worldwide, although this prevalence varies amongst different ethnicities [4].
The most common congenital deficiencies occur due to changes in the red and green cones. These are coded on the x-chromosome [5]. The genetic code for red and green cones is nearly identical and so the cones are easily changed to have the same or similar sensitivities.
Acquired defects are present in 10-20% of the population, increasing in prominence with age [6][7]. As these are not x-linked, acquired colour vision deficiencies are equally represented in both males and females.
What causes colour vision deficiency?
Colour vision deficiencies are caused by damaged, missing or altered photoreceptors in the eye, or by changes to the visual pathway, or brain areas responsible for processing colour vision. Deficiencies can be classified as either congenital or acquired.
Congenital colour vision deficiency
Congenital colour vision deficiencies (present at birth) are what most people think of when they use the term colour blindness. These are caused by genetic changes to the cones and are therefore usually the same in both eyes and stable over time. These genetic changes can cause effectively no functional cones (achromatopsia), one functional cone (monochromacy), two cones (dichromacy), or three cones but with altered sensitivity in one of the cones (anomalous trichromacy) [8].
If the cone is missing or not working there is no input from that cone type into the colour channel in the visual pathway to make the colour discrimination. If the cone is altered it will have a peak sensitivity closer to the neighbouring cone thus reducing the differential input available to make the colour differentiation. These are classified depending on which cone type is affected:
- Red cone: protan defect
- Green cone: deutan defect
- Blue cone: tritan defect
Acquired colour vision deficiency
Acquired colour vision deficiencies can be caused by anything that disrupts the cones, the visual pathway (the colour channels) along which colour information is carried, or the brain regions responsible for processing colour after birth [9]. Causes include eye diseases, systemic diseases, brain trauma and medications (see Table 1 for example causes). The type and severity of the defect caused can change over time (including the same cause producing different types of defects) and it is common for one eye to be affected more than the other.
Table 1. Examples of acquired colour vision deficiency causes. (Note this is not an exhaustive list.)
| Eye conditions | Systemic Diseases | Medications | Intracranial Injuries |
| Glaucoma [10] | Diabetes [11] | Chloroquine [12] | Traumatic brain injury [13] |
| Optic neuritis [14] | Multiple sclerosis [15] | Phenothiazines [16] | |
| Macular degeneration [17] | Parkinson’s disease [18] | Digoxin [19] | |
| Central serous retinopathy [20] | Alzheimer’s disease [21] | Ethambutol [22] |
Signs and symptoms of colour vision deficiencies
There are no outward signs of colour vision deficiency. Symptoms may include difficulty differentiating between colours, confusing colours or vision may appear washed out.
If you experience any of these symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How are colour vision deficiencies diagnosed?
Colour vision deficiencies can be diagnosed and managed by eye care practitioners, although screening for colour vision deficiencies by other health care workers such as the school nurse is common. The practitioner will ask about family eye history, previously diagnosed eye conditions, systemic conditions, general health and medications.
If risk factors for a colour vision deficiency are identified, tests to detect and diagnose a colour vision deficiency will be performed. In most cases, detection requires people to read numbers or identify shapes which are a different colour to the background (examples are given in Figure 4 and Figure 8).
Following on from this, the person may be asked to arrange coloured caps, match different lights, name the colour of lights (Figure 6) or indicate the direction of different colours on a screen in order to come to a complete diagnosis [27].
Ishihara test
Ishihara is a common colour vision screening test in which the task is to identify the number on the plate.

Farnsworth D15 colour test
The D15 test commonly used for acquired defects and for defining severity in congenital colour vision deficiencies. In this test, people are required to correctly order the caps starting from a reference cap. The colours that are mixed up here are used to determine the type of defect. A range of these tests in varying levels of difficulty can be used to determine severity of the colour vision deficiency.

Optec 900 lantern
The Optec 900 lantern is commonly used for testing in occupations that require signal light discrimination. In this task, the lights are displayed for 2.5 seconds and the person is required to correctly determine the colour of the top and bottom lights.

Can colour vision deficiencies be treated or cured?
Acquired colour vision deficiencies are treated by managing the underlying cause. There are no current treatments or cures for congenital colour vision deficiency, although investigations into gene therapy for congenital achromatopsia are underway [28].
Impact of living with a colour vision deficiency
The impact of colour vision deficiency depends on the severity. Some people with congenital colour vision deficiencies, particularly those with mild defects do not discover they have a colour vision deficiency until later in life [29].
The majority of people with congenital colour vision deficiency have 3 cones with 1 cone functioning with an altered sensitivity (anomalous trichromats). Their ability to discriminate different colours can vary from close-to-a person without colour vision deficiency if the affected cone has only a small shift in sensitivity, right through to functioning effectively as if only two cones were present.
Much of our world is colour-coded, and colour is commonly used for communication right from early learning at school, through to signalling in the transport industry, to coding in nature, for example ripe fruit. Colour vision deficiencies can have a significant impact on driving, occupation choice, and daily living including watching sport, recognising skin rashes and sunburn, and selecting appropriate clothes combinations [29] [30]. People with a colour vision deficiency may be unreliable when colour naming is used to identify an object and depending on severity may be slower to search a scene or visual display [31].
A range of occupations have colour vision standards either as a requirement of the job or for safety reasons including aviation, railway, maritime, police, fire, fine art and photography. Colour vision standards generally do not preclude all people with a colour vision deficiency but set a minimum colour discrimination standard. As colour is such a large influence in our world an accurate diagnosis is important so that colour vision deficiencies impact can be managed.
Colour vision deficiencies can impact clothing choices, and food choices, for example determining if meat is cooked. Within classrooms, having the teacher be aware that the child has a colour deficiency can avoid them being labelled as a naughty child simply for confusing colours, for example colouring people green rather than light pink (Figure 7). Awareness as early as possible is encouraged as management strategies are available [32] for classroom learning and appropriate occupational choices can be made.

Driving is a topic that should be discussed with patients who have a protan type defect as altered or missing long wavelength cones results in reduced sensitivity to red lights, such as stop or tail-lights [33]. Signal lights can also be confused with street lights. People with colour vision deficiencies have reported preferring day time driving as they have difficulty identifying reflectors on the road and rear stop lights on other cars [34].
Acquired colour vision deficiency is often managed differently to congenital colour vision deficiency. Acquired deficiencies can vary over time and so management consists of discussing things to be aware of with patient. For example, stop lights during driving are in a specific position and so this positional cue can be used to determine what the signal is. This requires awareness, as the usual colour cue may be diminished requiring patients to actively gather information from other cues.
Managing colour vision deficiencies
A range of lenses are commercially available and marketed to those with congenital colour vision deficiencies. These lenses typically remove part of the light spectrum coming to the observer resulting in less colours being able to be seen. The lenses may aide some patients with a colour vision deficiency by creating a lightness cue [35]. For example, if a person cannot distinguish between red and green, by using a red filter the green item will appear significantly darker (see Figure 8), and thus the person will be able to distinguish between the items based on brightness.
These lenses can be worn on just one eye, and people with a colour vision deficiency are able to learn how to distinguish between different colours based on the input to each eye. For some colours, this will create a flicker in intensity, seen as a shimmer, as the brain tries to combine the images from each eye. These filters do not return normal colour perception but create a mechanism to distinguish different colours. This is a learned response and so distinguishing different colours with these filters will be slower than for a person without colour vision deficiency.
For tests based on equal lightness, (for example the figure and background of the Ishihara) these may be helpful to break the camouflage effect these tests are based on, which may be incorrectly perceived as a return of colour vision (Figure 8). These lenses alter the perceived colour and do not help with discriminating between fine shades of colour as the changes in lightness or darkness of the image that are able to be created are small (Figure 8) [35].

DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- J. L. Schnapf, T. W. Kraft, and D. A. Baylor, “Spectral sensitivity of human cone photoreceptors,” Nature, vol. 325, no. 29, pp. 439–441, 1987, doi: 10.1038/325439a0.
- P. Lennie and J. A. Movshon, “Coding of color and form in the geniculostriate visual pathway,” J. Opt. Soc. Am. A, vol. 22, no. 10, p. 2013, 2005, doi: 10.1364/josaa.22.002013.
- S. G. Solomon and P. Lennie, “The machinery of colour vision,” Nat. Rev. Neurosci., vol. 8, no. 4, pp. 276–286, 2007, doi: 10.1038/nrn2094.
- M. P. Simunovic, “Colour vision deficiency,” Eye, vol. 24, no. 5, pp. 747–755, 2010, doi: 10.1038/eye.2009.251.
- M. P. Simunovic, “Acquired color vision deficiency,” Surv. Ophthalmol., vol. 61, no. 2, pp. 132–155, 2016, doi: 10.1016/j.survophthal.2015.11.004.
- D. Poinoosawmy, S. Nagasubramanian, and J. Gloster, “Colour vision in patients with chronic simple glaucoma and ocular hypertension,” Br. J. Ophthalmol., vol. 64, no. 11, pp. 852–857, 1980, doi: 10.1136/bjo.64.11.852.
- R. Lakowski, P. A. Aspinall, and P. R. Kinnear, “Association between colour vision losses and diabetes mellitus,” Ophthalmic Res., vol. 73, no. 4, pp. 145–159, 1972.
- D. F. Ventura et al., “Color vision loss in patients treated with chloroquine,” Arq. Bras. Oftalmol., vol. 66, no. 5 SUPPL., pp. 9–15, 2003, doi: 10.1590/S0004-27492003000600002.
- B. D. Greenwald, N. Kapoor, and A. D. Singh, “Visual impairments in the first year after traumatic brain injury,” Brain Injury, vol. 26, no. 11. pp. 1338–1359, 2012, doi: 10.3109/02699052.2012.706356.
- B. Katz, “The dyschromatopsia of optic neuritis: A descriptive analysis of data from the optic neuritis treatment trial,” Trans. Am. Ophthalmol. Soc., vol. 93, pp. 685–708, 1995.
- E. H. Martínez-Lapiscina et al., “Colour vision impairment is associated with disease severity in multiple sclerosis,” Mult. Scler. J., vol. 20, no. 9, pp. 1207–1216, 2014, doi: 10.1177/1352458513517591.
- R. Scott, G. T. Cunningham, J. M. Puddle, J. D. Klinger, and R. J. Jacobs, “Ocular side effects of phenothiazines,” Clin. Exp. Optom., vol. 74, no. 1, pp. 11–14, 1991, doi: 10.1111/j.1444-0938.1991.tb04601.x
- G. B. Arden and J. E. Wolf, “Colour vision testing as an aid to diagnosis and management of age related maculopathy,” Br. J. Ophthalmol., vol. 88, no. 9, pp. 1180–1185, 2004, doi: 10.1136/bjo.2003.033480.
- J. Birch, R. U. Kolle, M. Kunkel, W. Paulus, and P. Upadhyay, “Acquired colour deficiency in patients with Parkinson’s disease,” Vision Res., vol. 38, no. 21, pp. 3421–3426, 1998, doi: 10.1016/S0042-6989(97)00398-2.
- J. G. Lawrenson, C. Kelly, A. L. Lawrenson, and J. Birch, “Acquired colour vision deficiency in patients receiving digoxin maintenance therapy,” Br. J. Ophthalmol., vol. 86, no. 11, pp. 1259–1261, 2002, doi: 10.1136/bjo.86.11.1259.
- T. Bek and M. Kandi, “Quantitative anomaloscopy and optical coherence tomography scanning in central serous chorioretinopathy,” Acta Ophthalmol. Scand., vol. 78, no. 6, pp. 632–637, 2000, doi: 10.1034/j.1600-0420.2000.078006632.x.
- V. Polo et al., “Visual dysfunction and its correlation with retinal changes in patients with Alzheimer’s disease,” Eye, vol. 31, no. 7, pp. 1034–1041, 2017, doi: 10.1038/eye.2017.23.
- B. C. P. Polak, M. Leys, and G. H. M. van Lith, “Blue-yellow colour vision changes as early symptoms of ethambutol oculotoxiticty,” Ophthalmologica, vol. 191, pp. 223–226, 1985, doi: 10.1159/000309592.
- J. Birch, “Worldwide prevalence of red-green color deficiency.” J Opt Soc Am A Opt Image Sci Vis, Vol. 29, no. 3, pp. 313-20, 2012, doi: 10.1364/JOSAA.29.000313.
- J. Nathans, T. P. Piantanida, R. L. Eddy, T. B. Shows, and D. S. Hogness, “Molecular Genetics of Inherited Variation in Human Color Vision,” Science, vol. 232, no.4747, pp. 203-210, 1986, doi: 10.1126/science.3485310.
- E. Jafarzadehpur et al., “Color vision deficiency in a middle-aged population: the Shahroud Eye Study,” Int. Ophthalmol., vol. 34, no. 5, pp. 1067–1074, 2014, doi: 10.1007/s10792-014-9911-2.
- M. E. Schneck, G. Haegerstrom-Portnoy, L. A. Lott, and J. A. Brabyn, “Comparison of Panel F-15 Tests in a Large Older Population,” Optom Vis Sci, vol. 91, no. 3, pp. 284–290, 2014, doi: 10.1097/OPX.0000000000000152.
- S. J. Dain, “Clinical colour vision tests,” Clin. Exp. Optom., vol. 87, no. 4–5, pp. 276–293, 2004, doi: 10.1111/j.1444-0938.2004.tb05057.x.
- M. D. Fischer et al., “Safety and Vision Outcomes of Subretinal Gene Therapy Targeting Cone Photoreceptors in Achromatopsia: A Nonrandomized Controlled Trial,” JAMA Ophthalmol., vol. 138, no. 6, pp. 643–651, 2020, doi: 10.1001/jamaophthalmol.2020.1032.
- J. M. Steward and B. L. Cole, “What do color vision defectives say about everyday tasks?,” Optom. Vis. Sci., vol. 66, no. 5, pp. 288–295, 1989, doi: 10.1097/00006324-198905000-00006.
- B. L. Cole, “Impact of congenital colour vision deficiency: congenital colour vision deficiency does cause problems,” BMJ, vol. 330, no. 7482, p. 96, 2005, doi: 10.1136/bmj.330.7482.96.
- B. L. Cole, “The Handicap of Abnormal Colour Vision,” Aust. J. Optom., vol. 55, no. 8, pp. 304–310, 1972, doi: 10.1111/j.1444-0938.1972.tb06271.x.
- L. R. Prieto, Z. D. Siegel, and D. J. Kaiser, “One Fish, Two Fish; Red Fish (or Green Fish?): Assisting Students With Color Vision Deficiency,” Teach. Psychol., vol. 48, no. 1, pp. 90–94, 2021, doi: 10.1177/0098628320959946.
- B. L. Cole, “Protan colour vision deficiency and road accidents,” Clin. Exp. Optom., vol. 85, no. 4, pp. 246–253, 2002, doi: 10.1111/j.1444-0938.2002.tb03045.x.
- A. Tagarelli, A. Piro, G. Tagarelli, P. B. Lantieri, D. Risso, and R. L. Olivieri, “Colour blindness in everyday life and car driving,” Acta Ophthalmol. Scand., vol. 82, no. 4, pp. 436–442, 2004, doi: 10.1111/j.1395-3907.2004.00283.x.
- J. K. Hovis, “Long wavelength pass filters designed for the management of color vision deficiencies,” Optom. Vis. Sci., vol. 74, no. 4, pp. 222–230, 1997, doi: 10.1097/00006324-199704000-00024.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
