Endophthalmitis
Endophthalmitis – Written by Alexandre Lachance, MD-MSc candidate in supervision by Dr Ali Dirani, MD, MSc, MPH.
What is endophthalmitis?
Endophthalmitis is an inflammation of the tissue and/or the fluids inside the eye. It is a medical emergency that needs to be assessed by an ophthalmologist (medical doctor trained in subspeciality of the eyes) urgently. If not treated immediately, endophthalmitis can result in an irreversible loss of vision.
The following sections will briefly outline the global problem of endophthalmitis, its causes, the different types of endophthalmitis, its signs and symptoms, and some insights into its treatment.
How many people are affected by endophthalmitis?
Each year, over 3 million cases of cataract surgery is performed in the United States in which approximately 1,200 to 3,000 cases of acute postoperative endophthalmitis arise. [3-5] Endophthalmitis rates are different among regions of the world, surgical centres and populations. This disease is rare in developed countries and this may be attributed to the prevention during surgical procedures to reduce the risk of postoperative endophthalmitis. However, this disease is a medical emergency because it can have very devastating and potentially blinding effects on vision, if not addressed quickly.
Additionally, the economic aspect due to endophthalmitis following cataract surgery should not be overlooked. In the United States, between 2010 and 2014, the ophthalmic reimbursements by a health insurance company for cataract surgery with postoperative development of endophthalmitis were US$3,002 higher (156% greater) than cases with no development of endophthalmitis. [5]
What causes endophthalmitis?
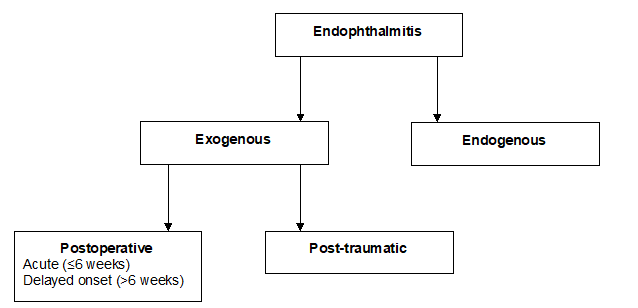
Endophthalmitis can be sterile or infectious. Infectious is further categorized into endogenous (originates from within the body) or exogenous (acquired externally).
Types of endophthalmitis
Sterile endophthalmitis
In sterile endophthalmitis, the inflammation results from an allergic reaction due to a medication injected in the eye, such as an anti-vascular endothelial growth factor (used in treatment of age-related macular degeneration or diabetic retinopathy), corticosteroid, triamcinolone or methotrexate.
Exogenous endophthalmitis
Exogenous endophthalmitis is more common than the endogenous form, with only 2-8% of all endophthalmitis attributed to endogenous cause. [1] In exogenous endophthalmitis, the causing pathogen is introduced from the external environment to the eyeball. The common causes are ocular surgery (e.g. cataract surgery or trabeculectomy), ocular trauma (open-globe injury), injection of medication in the eyeball or in some cases, from an external eye infection such as microbial keratitis. [2]
Endogenous endophthalmitis
In the endogenous form, the causing pathogen is originating from an infection in another part of the body (bacteria or fungemia) that spreads to the eyeball. For example, an infection of the heart (endocarditis) can spread through the blood to the eye.
The most frequent cause of endophthalmitis is intravitreal injections and cataract surgery. (exogenous).
What are the risk factors of endophthalmitis?
Endophthalmitis occurs at any age with no gender preference. The involvement of both eyes occurs in less than 25% of cases [6]
The main risk factors for exogenous endophthalmitis include blepharitis (eyelid inflammation), diabetes mellitus, older age, surgical complications and delayed wound closure. [7-12]
Endogenous endophthalmitis is frequently associated with predisposing conditions such diabetes mellitus, urinary tract infection, deficit of the immune system (human immunodeficiency virus (HIV)), renal failure and malignancies, intravenous drug use and recent hospitalization. [13]
The microorganisms involved in endophthalmitis depend on the type of endophthalmitis. Bacteria causes most cases of exogenous endophthalmitis while fungi are found typically in endogenous endophthalmitis. [14] The most frequent bacteria causing exogenous endophthalmitis are Staphylococcus and Streptococcus species. [15-16] The most frequent causing microorganisms of endogenous endophthalmitis are Candida albicans and Aspergillus species. [14]
What are the common signs and symptoms of endophthalmitis?
The main signs and symptoms are [17]:
- Decreased vision (generally within the first week after the surgery in cases of acute post-operative endophthalmitis)
- Eye pain
- Redness
- Hypopyon (accumulation of pus between the iris and the cornea)
Other signs and symptoms include [14, 18-22]:
- Swelling of the eyelid
- Floaters (small dark shapes that float across your vision)
- Photophobia (eye pain and discomfort to light)
- Corneal oedema (swelling of the transparent layer forming the front of the eye)
- Signs and symptoms of another infection (e.g. fever) in case of endogenous endophthalmitis
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is endophthalmitis diagnosed?
When there is any predisposing condition or a precipitating event, your eye doctor will examine your eyes closely and test your vision. The diagnosis of endophthalmitis is based on clinical presentation. Imaging studies (ultrasound or optical coherence tomography) can be performed to better assess the posterior part of your eyes. A sample of vitreous and/or aqueous humor (fluid in the eye) is carried out and then cultured to confirm the presence of microorganisms. The technique is called aqueous/vitreous tap, and it consists of inserting a tiny needle into your eye to remove a fluid sample [23]
Your doctor will also check for any underlying cause for endogenous endophthalmitis. Accordingly, some tests may be performed depending on your presentation, such as an echocardiogram (to rule out endocarditis), a urine culture (to rule out urinary tract infection), blood culture (infection in the blood) and/or chest X-ray (lung infection).
How is endophthalmitis treated?
The treatment consists of injecting antibiotic or antifungal agents inside the eye (intravitreal injection). In some cases, alongside the injection to the eye, intravenous (injected into the veins) antibiotic or antifungal agents are needed to control the endophthalmitis and to treat distant microorganisms in other parts of the body. Also, corticosteroids are sometimes used to decrease inflammation.
For severe cases with visual loss, a surgical operation called vitrectomy is done and it consists of removing the vitreous and replaced by gas or oil solution. [23] During the same surgery, a vitreous sample is carried out and is used for culture. At the end of the surgery, antibiotic or antifungal agents are injected in the eye.
The visual outcomes following adequate treatment are variable. In a large study, around 50% of patients with acute onset postoperative endophthalmitis had a final visual acuity of 20/40 or better. Early treatment of endophthalmitis is important to ensure good recovery of visual acuity. [24]
Once treatment is started, symptoms should improve within a 24 to 48 hours. [14] If you have no improvement after 48 hours or if your symptoms are worse, consult your eye doctor again.
Can I prevent endophthalmitis?
All precautions are undertaken during the surgical procedure to decrease the risk of endophthalmitis. Aseptic measures are rigorously followed such as use of povidone-iodine (betadine) and ocular antibiotic in ocular procedures to prevent microbial contamination.
To try to prevent endophthalmitis, it is important to
- Follow medical instructions after ocular procedures.
Consult your eye doctor if you have any suspicious symptoms after an ocular procedure.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- B.D. Novosad, and C.M. Callegan, “Severe bacterial endophthalmitis: towards improving clinical outcomes,” Expert Review Ophthalmology, vol. 5, no. 5, pp. 689-698, October 2010, doi: https://doi.org/10.1586/eop.10.52.
- N. Mamalis, “Endophthalmitis,” Journal of Cataract & Refractive Surgery, vol. 28, no. 5, pp. 729-730, May 2002, doi: https://doi.org/10.1016/S0886-3350(02)01350-0.
- J.K. Schmier et al., “An updated estimate of costs of endophthalmitis following cataract surgery among Medicare patients: 2010-2014,” Clinical Ophthalmololy, vol. 10, pp. 2121, October 2016, doi: https://doi.org/10.2147/OPTH.S117958.
- A. Haripriya, D.F. Chang, and R.D. Ravindran, “Endophthalmitis Reduction with Intracameral Moxifloxacin Prophylaxis: Analysis of 600 000 Surgeries,” Ophthalmology, vol. 124, no. 6, pp. 768-775, June 2017, doi: https://doi.org/10.1016/j.ophtha.2017.01.026.
- S. Pershing et al., “Endophthalmitis after Cataract Surgery in the United States: A Report from the Intelligent Research in Sight Registry,” Ophthalmology, vol. 127, no. 2, pp. 151-158, February 2020, doi: https://doi.org/10.1016/j.ophtha.2019.08.026.
- M.J. Greenwald, L.G. Wohl, and C.H. Sell, “Metastatic bacterial endophthalmitis: a contemporary reappraisal,” Survey of Ophthalmology, vol. 31, no. 2, pp. 81-101, September 1986, doi: https://doi.org/10.1016/0039-6257(86)90076-7.
- L. Keay et al., “Postcataract surgery endophthalmitis in the United States: analysis of the complete 2003 to 2004 Medicare database of cataract surgeries,” Ophthalmology, vol. 119, no. 5, pp. 914-922, May 2012, doi: https://doi.org/10.1016/j.ophtha.2011.11.023.
- W.V. Hatch et al., “Risk factors for acute endophthalmitis after cataract surgery: a population-based study,” Ophthalmology, vol. 116, no. 3, pp. 425-430, March 2009, doi: https://doi.org/10.1016/j.ophtha.2008.09.039.
- P. Lalitha et al., “Postcataract endophthalmitis in South India: incidence and outcome,” Ophthalmology, vol. 112, no. 11, pp. 1884-1889, November 2005, doi: https://doi.org/10.1016/j.ophtha.2005.05.020.
- E.S. West et al., “The incidence of endophthalmitis after cataract surgery among the U.S. Medicare population increased between 1994 and 2001,” Ophthalmology, vol. 112, no. 8, pp. 1388-1394, August 2005, doi: https://doi.org/10.1016/j.ophtha.2005.02.028.
- ESCRS Endophthalmitis Study Group, “Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors,” Journal of Cataract & Refractive Surgery, vol. 33, no. 6, pp. 978-988, June 2007, doi: https://doi.org/10.1016/j.jcrs.2007.02.032.
- H. Cao, L. Zhang, L. Li, and S. Lo, “Risk factors for acute endophthalmitis following cataract surgery: a systematic review and meta-analysis,” PLoS One, vol. 8, no. 8, pp. e71731, August 2013, doi: https://doi.org/10.1371/journal.pone.0071731.
- S.G. Schwartz et al., “Ocular Infection: Endophthalmitis,” Developments in Ophthalmology, vol. 55, pp. 176-188, October 2016, doi: https://doi.org/10.1159/000431195.
- K. Vaziri et al., S. Schwartz, K. Kishor, and H.W. Flynn Jr, “Endophthalmitis: state of the art,” Clinical Ophthalmology, vol. 9, pp. 95-108, January 2015, doi: https://doi.org/10.2147/OPTH.S76406.
- J. Sridhar et al., “Endophthalmitis caused by Klebsiella species,” Retina, vol. 34, no. 9, pp. 1875-1881, September 2014, doi: https://doi.org/10.1097/IAE.0000000000000162.
- J.J. Miller et al., “Endophthalmitis caused by Streptococcus pneumoniae,” American Journal of Ophthalmology, vol. 138, no. 2, pp. 231-236, August 2004, doi: https://doi.org/10.1016/j.ajo.2004.03.008.
- B. Doft, “Focal Points: Modules for Clinicians,” San Francisco: American Academy of Ophthalmology, Endophthalmitis Management, 1997.
- H.W. Lim et al., “Endogenous endophthalmitis in the Korean population: a six-year retrospective study,” Retina, vol. 34, no. 3, pp. 592-602, March 2014, doi: https://doi.org/10.1097/IAE.0b013e3182a2e705.
- M.I. Binder et al., “Endogenous endophthalmitis: an 18-year review of culture-positive cases at a tertiary care center,” Medicine (Baltimore), vol. 82, no. 2, pp. 97-105, March 2003, doi: https://doi.org /10.1097/00005792-200303000-00004.
- H. Zhang, and Z. Liu, “Endogenous endophthalmitis: a 10-year review of culture-positive cases in northern China,” Ocular Immunology and Inflammation, vol. 18, no. 2, pp. 133-138, April 2010, doi: https://doi.org/10.3109/09273940903494717.
- T.L. Jackson, T. Paraskevopoulos, and I. Georgalas, “Systematic review of 342 cases of endogenous bacterial endophthalmitis,” Survey of Ophthalmology, vol. 59, no. 6, pp. 627-635, June 2014, doi: https://doi.org/10.1016/j.survophthal.2014.06.002.
- V. Schiedler et al., “Culture-proven endogenous endophthalmitis: clinical features and visual acuity outcomes,” American Journal of Ophthalmology, vol. 137, no. 4, pp. 725-731, April 2004, doi: https://doi.org/10.1016/j.ajo.2003.11.013.
- M.A. Sadiq et al., “Endogenous endophthalmitis: diagnosis, management, and prognosis,” Journal of Ophthalmic Inflammation and Infection, vol. 5, no. 1, pp. 32, December 2015, doi: https://doi.org/10.1186/s12348-015-0063-y.
- Endophthalmitis Vitrectomy Study Group, “Results of the Endophthalmitis Vitrectomy Study: a randomized trial of immediate vitrectomy and of intravenous antibiotics for the treatment of postoperative bacterial endophthalmitis,” Archives of ophthalmology, vol. 113, no. 12, pp. 1479-1496, December 1995, doi: https://doi.org/10.1001/archopht.1995.01100120009001.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.

