Open angle glaucoma
Glaucoma – Written by Dr. Eamonn Fahy, MB, BCh, BAO, Ph.D.
What is glaucoma?
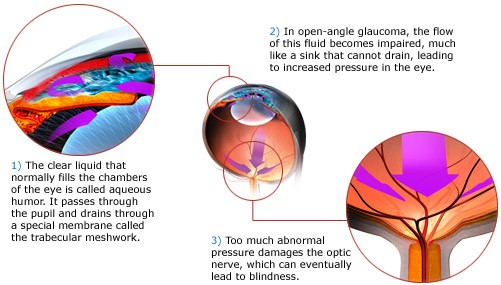
Glaucoma is an eye condition in which the optic nerve (essential bundle of nerve cells that carries visual signals from the eye to the brain) is damaged and peripheral vision is affected. In the early stages of glaucoma, there may be no symptoms. In the late stages, an individual may be left with only a small area of central vision (tunnel vision) or even blindness. There are two main categories of glaucoma: open angle glaucoma and angle closure glaucoma. The ‘angle’ refers to the drainage angle at the front of the eye which allows fluid to drain from the eye. In this article, we will discuss open angle glaucoma.
The following sections will briefly outline the public health implications of open angle glaucoma, causes of open angle glaucoma, its signs and symptoms, how it is diagnosed and some insights into its treatment.
The global problem of glaucoma
The global prevalence of open angle glaucoma is estimated to be 3.05%.[1] Glaucoma is the most frequent cause of irreversible vision loss worldwide.[2]
It is estimated that the number of people with glaucoma worldwide will increase by 74% between 2013 and 2040.[1] This increase is primarily due to an ageing global population, where the average age worldwide is increasing over time, as people live longer.
Glaucoma represents a significant economic burden, both in terms of treatment costs and the impact on an individual’s ability to work and lead a normal life. For example, the total cost of open angle glaucoma in Australia in 2005 was $AU1.9 billion and this is estimated to rise to $AU4.3 billion by 2025.[3]
Causes of open angle glaucoma
Open angle glaucoma comprises a group of conditions that have different causes. The two main causes for open angle glaucoma are increasing age and increased pressure inside the eye (intraocular pressure). However, younger people can be affected by glaucoma and the condition can also occur in people with normal intraocular pressures.
Primary open angle glaucoma
The most common type of open angle glaucoma is called primary open angle glaucoma. Primary open angle glaucoma does not have an identifiable underlying cause. However, there are risk factors for the condition which include:
Raised intraocular pressure
The unit used to measure intraocular pressure (IOP) is mmHg. A healthy reading of IOP is 10-21 mmHg, with an average of 15 mmHg.[4] IOP above 21 increase a person’s risk for developing glaucoma. However, glaucoma can occur with normal IOP too (see below ‘Normal tension glaucoma’).
Increasing age
The risk of glaucoma increases with increasing age. This risk increases with every decade over the age of 40.[1]
Ethnicity
People of African ancestry are at an increased risk of primary open angle glaucoma. People of Asian ancestry have an increased risk of angle closure glaucoma.
Myopia
Higher levels of myopia or short-sightedness, increase the risk of primary open angle glaucoma. It has been suggested that people with myopia exceeding -6D (high myopia) are most at risk.[5]
Family history
A family history of primary open angle glaucoma increases a person’s risk for the condition. This association is most important if a person’s siblings or parents are affected.[6]
Normal tension glaucoma
Normal tension glaucoma is where glaucoma occurs in the presence of normal IOP. It is not quite the same as primary open angle glaucoma, because there are different risk factors that may be contributory. These include: migraine, obstructive sleep apnea (when the muscles that support the soft tissues in the throat, such as the tongue and soft palate temporarily relax), cardiovascular disease or raynaud’s disease (short term interruption of blood flow to the extremities such as fingers and toes). Normal tension glaucoma is more common in people of Japanese ancestry.
Secondary open angle glaucoma
Secondary open angle glaucoma describes a group of conditions where there is an underlying cause for increased IOP which then goes on to cause glaucoma.
Some underlying causes for secondary open angle glaucoma include:
Inflammation
Inflammation inside the eye, or uveitis, can cause increased IOP and glaucoma.
Steroid medication
The use of steroid medication as eye drops or tablets can cause increased IOP in some people, also referred to as a ‘steroid response’.
Trauma
Trauma to the eye can damage the drainage system of the eye and can cause increased IOP and glaucoma.
Pigmentary glaucoma
Some individuals have a different shape of anatomy at the front of the eye which can cause release of pigment from the iris (the coloured part of the eye), which can then block the drainage system of the eye and cause increased IOP.
Previous surgery
Surgery for a range of eye conditions can cause increased IOP which can cause glaucoma if the pressure remains elevated over a long period of time. Possible contributory surgeries include: retinal detachment surgery, corneal graft surgery, complicated cataract surgery, eye injections (for age related macular degeneration or diabetic eye disease).
What are the glaucoma symptoms?
About the glaucoma symptoms, in the early stages of glaucoma, there may be no symptoms. There may be very little, if any, damage to the peripheral vision and an individual may not be aware of any change to their vision. In the majority of cases of open angle glaucoma, there is no pain.
In the late stages of glaucoma, an individual may be left with only a small area of central vision (tunnel vision) or even blindness. Advanced glaucoma may also impact a person’s ability to visually adapt to darker environments, for example going from outside to inside a building. In late stages of the disease, a person’s ability to navigate around their home or other environments may be severely impaired.

If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye diseases may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How can open angle glaucoma progress?
Glaucoma begins with mild imperceptible damage to a person’s peripheral vision and can progress to blindness if left untreated. The rate of progression is usually slow and takes years to become symptomatic and impact on visual function. However, once peripheral vision is lost, it cannot be regained. The goal of treatment is to slow down the progression of glaucoma to a point where it does not impact significantly on a person’s vision or quality of life within their lifetime.
How is open angle glaucoma diagnosed?
Open angle glaucoma is diagnosed by an eye health professional based on a comprehensive eye check. There is a combination of tests that are performed to diagnose glaucoma, of which, the most important of these tests are:
Measurement of intraocular pressure
This can be performed with several different machines, including handheld devices and larger instruments.
Visual field test
This refers to a test in which peripheral vision is examined using a visual field machine. It involves pressing a button on a handheld device as lights are detected in a person’s peripheral vision.
Optic nerve examination
The optic nerve can be damaged by glaucoma and is examined by looking at the back of the eye using a slit lamp (a microscope) and by taking photos and scans of the nerve.
Other tests
Tests of visual acuity (reading a chart with letters), measurement of corneal thickness (using a small handheld device) and examining the drainage angles of the eye (using a contact lens) are other tests which can assist with diagnosing glaucoma.

Combining these tests with asking questions that are used to determine a person’s risk of glaucoma helps an eye health professional to make a diagnosis.
How is the glaucoma treatment?
The main glaucoma treatment is to lower the IOP by using medication (eye drops), laser or surgery. Treatment for glaucoma cannot cure the condition, but the goal is to slow the progression of glaucoma so that it does not affect a person’s visual function within their lifetime. There are three main ways to treat glaucoma: medications (eye drops), laser and surgery.
Medications
There are a number of different medications in the form of eye drops which can be used by people on a daily basis to reduce IOP.
Laser
Selective laser trabeculoplasty (SLT) is a laser procedure which can be used to lower IOP.[7] It is painless, takes about 5-10 minutes per eye and is performed in the outpatient clinic. SLT targets the drainage angles of the eye to increase drainage of fluid from the eye.
Surgery
In the later stages of glaucoma or in people with very elevated IOP, surgery may be an option to reduce the IOP and slow the progression of damage to the vision. The two main types of surgery are called the trabeculectomy and tube shunt surgery. There are other devices which can be surgically implanted to reduce IOP (minimally invasive glaucoma surgery, MIGS), but they may not be as effective at lowering IOP as the trabeculectomy or tube shunt surgery.
Can open angle glaucoma be prevented?
Primary open angle glaucoma cannot be prevented from occurring. However, with early detection and treatment, the rate of progression of glaucoma can be slowed to a point whereby a person may not be symptomatic or may only have mild impact on their visual function.
The earlier glaucoma is detected and treatment started, the less likely it is for a person to be impacted by the condition. For this reason, all adults 50 years or older should attend an eye health professional every 2 years for a comprehensive eye exam. People who have a family history of glaucoma or are of African or Asian descent should attend every 2 years from the age of 40.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- Y. C. Tham et al., “Global prevalence of glaucoma and projections of glaucoma burden through 2040: a systematic review and meta-analysis,” Ophthalmology, vol. 121, no. 11, pp. 2081-90, Nov 2014, doi: 10.1016/j.ophtha.2014.05.013
- R. R. A. Bourne et al., “Causes of vision loss worldwide, 1990–2010: a systematic analysis,”. The Lancet Global Health, vol. 1, no. 6, pp. 339-49, Dec 2013, doi: 10.1016/S2214-109X(13)70113-X.
- M. Dirani et al., “Economic impact of primary open-angle glaucoma in Australia,” Clin Exp Ophthalmol, vol. 39, no. 7, pp. 623-32, June 2011, doi: 10.1111/j.1442-9071.2011.02530.x.
- P. T. Khaw, P. Shah and A. R. Elkington. “Glaucoma–1: Diagnosis,” BMJ, vol. 328, no. 7431, pp. 97-9, Jan 2004, doi: 10.1136/bmj.328.7431.97.
- X. Liang et al., “High myopia and glaucoma susceptibility the Beijing Eye Study,” Ophthalmology, vol. 114, no. 2, pp. 216-20, Feb 2007, doi: 10.1016/j.ophtha.2006.06.050.
- J. M. Tielsch et al., “Family history and risk of primary open angle glaucoma. The Baltimore Eye Survey,” Arch Ophthalmol, vol. 112, no. 1, pp. 69-73, Jan 1994, doi: 10.1001/archopht.1994.01090130079022.
- G. Gazzard et al., “Selective laser trabeculoplasty versus eye drops for first-line treatment of ocular hypertension and glaucoma (LiGHT): a multicentre randomised controlled trial,” The Lancet, vol. 393, no. 10180, pp. 1505-16, doi: 10.1016/S0140-6736(18)32213-X
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
