Herpes Zoster Ophthalmicus
Herpes zoster ophthalmicus – Written by Dr. Eamonn Fahy, MB, BCh, BAO, Ph.D.
What is herpes zoster ophthalmicus?
Herpes zoster ophthalmicus is commonly known as shingles that occurs around the eye. Shingles is a reactivation of the varicella zoster virus, which is the virus that causes chickenpox.
After people have chickenpox as children, the virus remains inactive in the nerves that supply the skin. The varicella zoster virus can reactivate later in life and can travel along these nerves to cause a blistering rash on the skin.
A shingles rash can occur anywhere on the skin. When it occurs around the eye, it is called herpes zoster ophthalmicus. Sometimes the rash will occur on the skin around the eye but the eye itself is unaffected. In some people, different parts of the eye can become affected by reactivation of the varicella zoster virus.
In people who have been immunised against chickenpox, and who never had chickenpox as a child, there is still a risk of developing shingles.
The following overview will cover the economic costs of herpes zoster ophthalmicus, its causes, its different categories, its common signs and symptoms, the progression of the condition, methods of diagnosis, treatment options, and prevention.
How common is herpes zoster ophthalmicus?
Shingles will affect 20 to 30% of people at some point in their lifetime, and of these people who develop shingles, 10 to 20% will have herpes zoster ophthalmicus [1].
Shingles represents a significant economic burden and in a recent study was estimated to cost the United States healthcare system US$ 2.4 billion annually in direct medical costs and productivity losses [2].
Causes of herpes zoster ophthalmicus
As described above, herpes zoster ophthalmicus is caused by reactivation of the varicella zoster (chickenpox) virus along the nerves that supply the skin around the eye, causing a blistering rash in this region.
In many cases, there is no clear trigger for the onset of the condition. In other cases, there are risk factors which increase the chance of developing the condition.
These risk factors include:
- Increasing age is a risk factor as shingles is most common in people over 50 years old
- People undergoing treatment for cancer for example, chemotherapy or radiotherapy
- People taking immunosuppressive medications for example, people taking medications to prevent rejection of organ transplants
- Immunocompromised patients for example, people with untreated HIV (human immunodeficiency virus)
What are the categories of herpes zoster ophthalmicus?
Eye involvement in herpes zoster ophthalmicus can be categorised by the part of the eye which is affected. The following structures of the eye may be involved:
- Conjunctivitis: Infection or inflammation of the conjunctiva, the outer layer that lines the eyelid and eyeball.
- Blepharitis: Inflammation of the eyelids
- Keratitis: Ulcers involving the cornea
- Uveitis: Inflammation inside the eye
- Rarely, more severe eye involvement can occur whereby the retina (retinitis), optic nerve (optic neuritis), or the muscles controlling eye movement (cranial nerve palsies) are affected
What are the common signs and symptoms of herpes zoster ophthalmicus?
Herpes zoster ophthalmicus causes a blistering rash on the skin around the eye. This rash usually occurs above the eye and can extend up to the scalp. The rash can only affect one side of the face at a time. Initially the blisters are fluid filled and later they break open and crust over.
Prior to the rash, it is common to experience sensations of pain, burning, and sensitivity in the affected area.
Up to 85% of the affected people will experience symptoms relating to eye involvement [3], in addition to the rash. These symptoms may include:
- Red eye
- Painful eye
- Reduced vision
- Light sensitivity
- Excessive tearing
- Gritty sensation or feeling of something in the eye
Up to 47% of people will experience ongoing pain in the affected region after the rash has resolved [1]. This condition is called postherpetic neuralgia.
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How can herpes zoster ophthalmicus progress?
In most cases the rash resolves within 2 weeks, and in some cases may take 4 to 6 weeks to resolve. Eye involvement is often mild and is usually resolved within a similar time period. In some cases, the eye involvement can be more severe and can take months to resolve.
If untreated, herpes zoster ophthalmicus has a higher risk of eye involvement and of postherpetic neuralgia.
If eye involvement is untreated, sight threatening complications such as glaucoma, cataract, or corneal scarring can occur.
How is herpes zoster ophthalmicus diagnosed?
Herpes zoster ophthalmicus can be diagnosed by a healthcare professional and treatment can be initiated in the community hospitals, for example by your local family doctor.
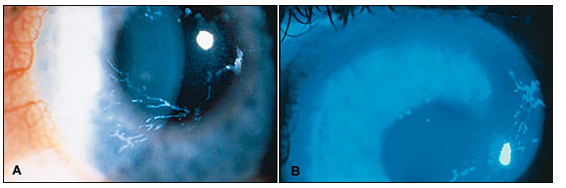
Eye involvement in herpes zoster ophthalmicus is diagnosed by an eye health professional based on a comprehensive eye check. The most important component of this is the slit lamp examination, where a microscope is used to look at the eye. An orange stain called fluorescein may be used to detect ulcers which can occur on the cornea (the clear outer layer at the front of the eye).
The comprehensive eye check also includes looking at structures at the back of the eye such as the retina and involves dilating the pupils (making the pupils big) with eye drops.
A swab may be taken of the rash to confirm the diagnosis, but this is not always necessary.
Other investigations such as a scan of the back of the eye using optical coherence tomography (OCT) scan may be used to see certain parts of the eye in more detail.
How is herpes zoster ophthalmicus treated?
Herpes zoster ophthalmicus is treated using oral antiviral medication (tablets). Treatment is most effective if commenced within 72 hours from the development of the rash.
Treatment for eye involvement depends on the severity of involvement and may include lubricant eye drops (mild eye involvement) or steroid eye drops (more severe eye involvement).
Pain associated with herpes zoster ophthalmicus can be managed with oral pain medication.
Can herpes zoster ophthalmicus be prevented?
Herpes zoster vaccination is currently available and is 89.1% effective against herpes zoster ophthalmicus [4]. The vaccine is usually offered to people over the age of 50 years or those who are otherwise at risk of developing shingles, for example in immunocompromised people. This vaccine is different to the vaccine used to immunise people against chickenpox.
Starting antiviral treatment within 72 hours of the onset of the rash reduces the risk of eye involvement and postherpetic neuralgia.
You cannot transmit shingles to other people; however, it is possible to transmit chickenpox to people who have never had chickenpox or have not been vaccinated against chickenpox. This is caused by the spread of the varicella zoster virus from the blistering rash.
Because of this risk of transmitting chickenpox, people with shingles (and herpes zoster ophthalmicus) are advised to avoid contact with people who have not had chickenpox in the past or who have been vaccinated against chickenpox, particularly immunocompromised people or pregnant women, in whom chickenpox could be associated with severe diseases.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- Liesegang, T. J. Herpes zoster ophthalmicus natural history, risk factors, clinical presentation, and morbidity. Ophthalmology 115, S3–12 (2008).
- Harvey, M., Prosser, L. A., Rose, A. M., Ortega-Sanchez, I. R. & Harpaz, R. Aggregate health and economic burden of herpes zoster in the United States: illustrative example of a pain condition. Pain 161, 361–368 (2020).
- Niederer, R. L., Meyer, J. J., Liu, K. & Danesh-Meyer, H. V. Herpes Zoster Ophthalmicus Clinical Presentation and Risk Factors for Loss of Vision. Am. J. Ophthalmol. 226, 83–89 (2021).
- Lu, A., Sun, Y., Porco, T. C., Arnold, B. F. & Acharya, N. R. Effectiveness of the Recombinant Zoster Vaccine for Herpes Zoster Ophthalmicus in the United States. Ophthalmology (2021) doi:10.1016/j.ophtha.2021.04.017.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.

