Hypermetropia
Hypermetropia – Written by Purrven Bajjaj, B Optom, MSc Clinical Optom.
What is hypermetropia?
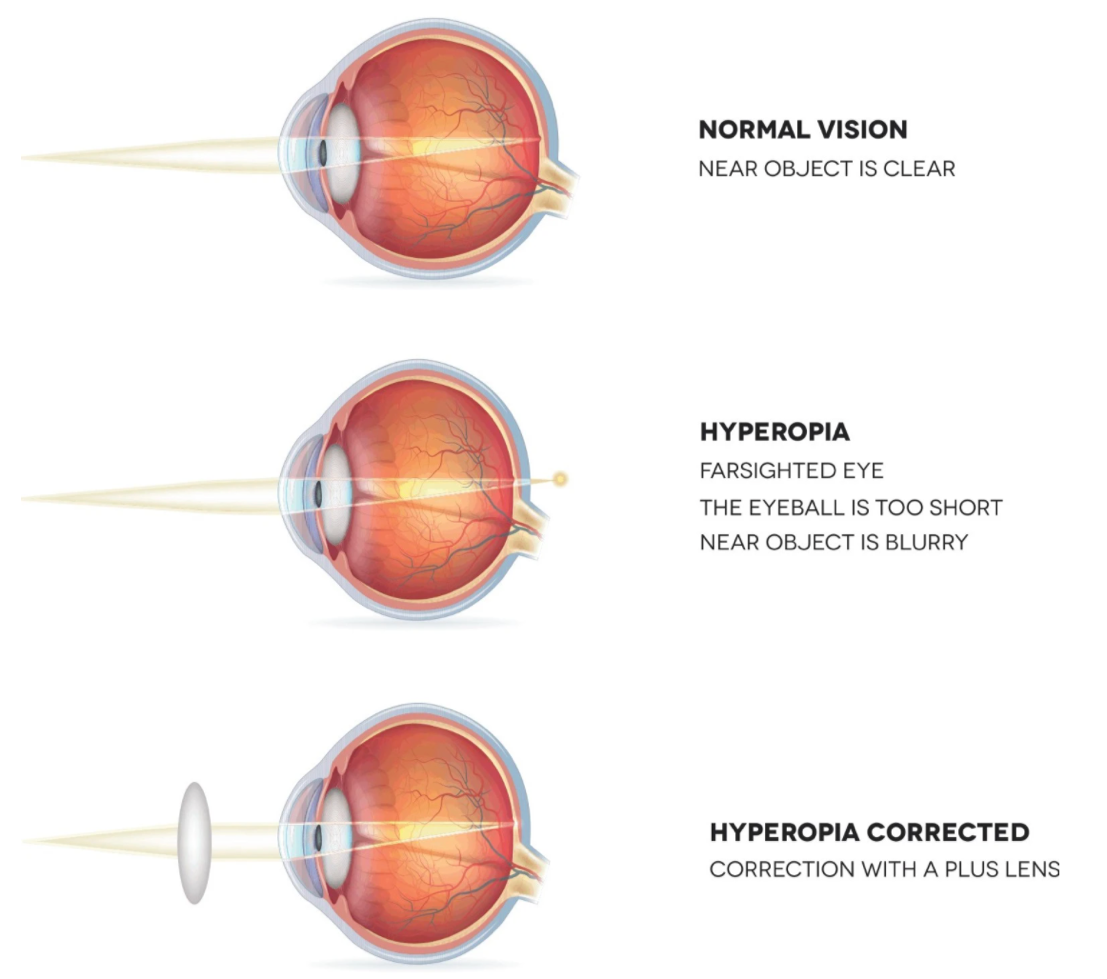
Hypermetropia occurs when the length of the eyeball is too short or the cornea (transparent layer at the front of the eye) is not curved enough to cause light to focus on the retina. As such, light rays entering the eye fall behind the retina (light sensitive tissue located at the back of the eye) instead of directly on the retina, causing blurry vision when looking at near objects.
Hypermetropia is also sometimes referred to as hyperopia or far-sightedness. It is the opposite of myopia (near-sightedness) where the length of the eyeball is too long, causing light to focus in front of the retina, which affects a person’s ability to see distant objects clearly.
This overview will cover the public health implications of hypermetropia, its causes, its common signs and symptoms, how it is diagnosed, and some insights into its management and treatment.
How common is hypermetropia?
Based on a study conducted in the United States (US) on children from 4 different ethnic groups aged 5 to 17 years old, it was reported that Caucasians have the highest rates of hypermetropia among the 4 ethnic groups, with close to 2 in 10 having hypermetropia. This was followed by the Hispanic group, with 1 in 10 having hypermetropia. Within this study population, it was also found that hypermetropia is less common in Asians and African Americans, with 6 in 100 in both groups having hypermetropia [1].
In adults, another US-based study reported that approximately 4 in 100 adults aged 20 years and above have hypermetropia [2].
The total prevalence of hypermetropia across all age groups is predicted to reach approximately 118 million people in the US by 2030. This means that a third of the US population is expected to have hypermetropia by 2030 and this number is expected to increase further to 142 million by the year 2050 [3].
The economic impact of hypermetropia
A recent (2018) study published in Iran reported that the economic burden of hypermetropia in Iran is approximately US$ 5.2 billion [4]. Global estimates of the direct and indirect costs of hypermetropia are still emerging, however it is known that uncorrected refractive errors in general can lead to loss of productivity-related costs. The global cost associated with the loss of productivity due to uncorrected refractive errors (myopia or short-sightedness, hypermetropia or far-sightedness, presbyopia, and astigmatism) has been estimated at US$ 244 billion per year [5].
What age does hypermetropia typically develop?
Hypermetropia can occur at any age. It typically starts from birth, with the level of hypermetropia decreasing as a child grows older through a process called emmetropisation, where the length of the eyeball aims to match the power of the eye.
A study done to analyze the refractive error or degree of the eye in children from birth till 5 years old showed that 9 in 10 full term infants (born after 39 weeks of pregnancy) have hypermetropia of +3.50D (dioptres) because their eyes are smaller. As the eyeball grows, the hypermetropia self corrects [6].
The process of emmetropisation differs among children. If the lowering of hypermetropia and the growth of the eyeball develops at a slower rate, this can result in hypermetropia after the eyeball growth is complete at around 8 to 9 years old.
What causes hypermetropia?
In hypermetropia, the length of the eyeball is too short, or the cornea (transparent layer protecting the front of the eyeball) is too flat. There is mounting evidence to support a genetic influence in the development of hypermetropia. Large scale studies from across the globe have shown that approximately 1 in 2 individuals with hypermetropia were also found to have at least 1 sibling or parent with hypermetropia [7].
Different severities of hypermetropia
Dioptres (D) is the unit used to measure the degree of the corrective lens required to achieve clear vision, in increments of 0.25D. A convex (outward curving) or plus lens is required to correct hypermetropia to focus the light rays onto the retina to produce clear vision. Hypermetropia is classified into 3 categories based on its severity:
| Mild hypermetropia | +0.50 to +2.00D |
| Moderate hypermetropia | +2.25 to +5.00D |
| High hypermetropia | More than +5.00D |
Signs and symptoms of hypermetropia
The common signs of symptoms of hypermetropia include:
- Blurry vision when doing near work activities like, reading, using digital devices, drawing, sewing or knitting
- Eye strain
- Headaches after focusing on something close up
- Tired eyes

The symptoms of hypermetropia can vary depending on its severity. Children and adults younger than 40 years old with mild hypermetropia (+0.50D to +2.00D) generally do not notice problems seeing because the accommodation in the eye is active and strong enough to overcome the far-sightedness. Accommodation refers to the focusing ability of our eyes to maintain clear vision at different distances.
People with moderate (+2.25D to +5.00D) and high (more than +5.00D) hypermetropia may notice blurry vision at near and far distances and tend to need corrective glasses at all times.
Hypermetropia is often confused with presbyopia, an age-related change in the eye in which the lens of the eyes become harder and less flexible. Ciliary muscles in the eye also become weaker with age. The ciliary muscles are a ring of smooth muscle in the eye that helps to control the shape of the eye lens when focusing on nearby and distant objects. The hardening of the eye’s lens and weakening of the ciliary muscles in people with presbyopia makes it difficult for the eye’s lens to adjust and have a clear image of nearby objects, such as reading a text message on the mobile phone. Hypermetropia can occur at any age while presbyopia typically occurs over in people aged 40 years and older.
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is hypermetropia diagnosed?
Hypermetropia is diagnosed by trained eye care professionals in a clinical setting through a comprehensive eye check. Vision will be tested by reading letters or numbers off a visual acuity chart known as a Snellen chart or a LogMAR chart up close (30 to 45 centimetres away from the eyes) or at a distance (3 or 6 metres away from the eyes).

In mild degrees of hypermetropia (+0.50D to +2.00D), vision at a distance and up close can sometimes be clear. As such, without regular comprehensive eye examinations, people with mild hypermetropia tend to go undetected. This is especially so in schoolchildren since vision tests done in schools only include a screening and refraction (a test done by an eye care professional where various lenses are compared to decide which lens produces clear vision) is not examined, resulting in undiagnosed cases of lower degrees of hypermetropia in some cases.
When doing a refraction test, the response of the patient is crucial. In some instances, especially among children when the understanding and ability to express what they see is still developing, an additional test called retinoscopy is done. A retinoscope is used to shine light into the eye to check how light bends in the eye.

Accommodation of the eye (focusing ability of our eyes to maintain clear vision at different distances) is active in children and young adults. The amount of accommodation can affect the results of the refraction test, making it appear lower or higher than it actually is. As such, cycloplegic eye drops that dilate the pupils and temporarily relax the ciliary muscles responsible for accommodation are used, allowing the eye care professional to do a cyclorefraction for an accurate degree check.
The combination and strength of cycloplegic drops vary according to specific country regulations. Cycloplegic drops will cause a temporary relaxation of the muscles used in accommodation and can result in blurring of vision. This blurring usually goes away, and vision will be regained to what it was before the drops were given within a few hours.
How is hypermetropia treated?
Hypermetropia is corrected with spectacles, contact lenses or refractive surgery. Spectacles or contact lenses may be always required or only when reading, using the computer or engaging in other close-up work.
Spectacles
In hypermetropia, plus or convex lenses are used to focus light rays that enter the eye onto the retina to correct vision. At moderate to high degrees (more than +2.25D) of hypermetropia, convex or plus lenses are used to enlarge the image, which may give rise to a magnified appearance of the spectacle lenses when worn.
There are 2 types of lenses when choosing spectacles, spherical and aspheric. Spherical lenses have the same curve across the entire surface of the lens, like a circle. Aspheric lenses have an oval shape, with a different curve across the entire surface of the oval lens, decreasing towards the edge. When choosing spectacles for hypermetropia of more than +2.25D, aspheric high index lenses are recommended as they are thinner, lighter, and the lens thickness is not as visible as compared to spherical lenses.
The index refers to the thickness of the lens, where higher index lenses are thinner and lower index lenses are thicker. An eye care professional will recommend the most suitable option based on the age, degree of hypermetropia, eye health, and visual requirements of the patient.
Contact lenses
Contact lenses are divided into 2 main categories, soft and hard. Soft lenses are the more common choice among contact lens wearers because they are flexible and are able to be moulded to the shape of the eye. The US Food and Drug Administration (FDA) regulates contact lenses as a medical device. It is important for contact lens users to maintain good contact lens care and hygiene to prevent eye infections and other contact lens-related eye problems. Routine eye checks with an eye care professional are also essential. Seek prompt medical attention when experiencing discomfort, soreness, itching, and redness of the eye from wearing contact lenses.
Refractive surgery

Refractive surgery is when a surgeon applies a laser to the cornea (transparent layer protecting the surface of the eye) to change the way light enters the eye, so that it is focused on the retina (back portion of the eye) to produce clear vision. Common refractive surgeries include laser-assisted in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK).
LASIK is the most common type of refractive surgery and involves creating a thin flap on the surface of the cornea. A laser then removes a precise amount of tissue from the inner layers of the cornea needed to change its shape for clear vision. The flap is then placed back into its original position to heal. In PRK, lasers remove a thin layer of tissue from the surface of the cornea instead in order to flatten its shape, which helps to refocus incoming light onto the retina.
As per FDA recommendations, refractive surgeries should only be performed on those aged 18 years and older. The eligibility and type of refractive surgery are dependent on the patient’s general health and the results of a comprehensive eye check that includes additional tests that are not done routinely to get an accurate assessment of the cornea (transparent layer protecting the surface of the eye).
Hypermetropia and its complications
Hypermetropia can lead to other complications such as the development of other more serious eye conditions if left uncorrected and untreated. Infants with hypermetropia of +3.50D or higher are 13 times more likely to develop strabismus by the age of 4 years if left uncorrected [8]. Strabismus develops when both eyes are not coordinating with one another, and both eyes do not look at the same place at the same time. Over time, the weaker eye may get ignored by the brain due to the lack of reception, leading to amblyopia or lazy eye.
In one study, it was reported that children older than 6 years with hypermetropia of more than +3.25D have an 18 times higher risk of developing amblyopia [9]. Amblyopia and strabismus during infancy and early childhood (less than 4 years old) can disrupt a child’s visual development [10].
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- R. N. Kleinstein et al., “Refractive Error and Ethnicity in Children,”. Arch Ophthalmol, vol. 121, no. 8, pp. 1141-7, Aug 2003, doi: 10.1001/archopht.121.8.1141.
- S. Vitale, L. Ellwein, M. F. Cotch, F. L. Ferris 3rd, and R. Sperduto, “Prevalence of refractive error in the United States, 1999-2004,” Arch. Ophthalmol. (Chicago, Ill. 1960), vol. 126, no. 8, pp. 1111–1119, Aug. 2008, doi: 10.1001/archopht.126.8.1111.
- National eye institute: Far sightedness data and statistics. (2019).
- S. F. Mohammadi et al., “Refractive surgery: the most cost-saving technique in refractive errors correction,” Int J Ophthalmol, vol. 11, no. 6, pp. 1013-1019, Jun 18 2018, doi: 10.18240/ijo.2018.06.20
- K. S. Naidoo et al., “Potential lost productivity resulting from the Global Burden of Myopia,” Ophthalmology, vol. 126, no. 3, pp. 338-346, Mar 2019, doi: 10.1016/j.ophtha.2018.10.029
- A. Kuo, R. B. Sinatra and S. P. Donahue “Distribution of refractive error in healthy infants,” J AAPOS, vol. 7, no. 3, pp. 174-7, Jun 2003, doi: 10.1016/s1091-8531(03)00017-x
- D. Stambolian “Genetic Susceptibility and Mechanisms for Refractive Error,” Clin Genet, vol. 84, no. 2, pp. 102-108, Jun 10 2013, doi: 10.1111/cge.12180
- St Louis, “Clinical Practice Guideline: Care of the Patient with Hyperopia”. American Optometric Association. 1997.
- E. E. Birch and J. Wang, “Stereoacuity outcomes after treatment of infantile and accommodative esotropia,” Optom Vis Sci, vol. 86, no. 6, pp. 647-52, June 2009, 10.1097/OPX.0b013e3181a6168d
- M. T. Kulp., et al., “Relationship of Hyperopia with Amblyopia, Strabismus and Stereoacuity in Preschool Children,” Invest Ophthalmol Vis Sci, vol. 53, no. 14, pp. 153, 2012
- J. M. Ip et al., “Prevalence of hyperopia and associations with eye findings in 6 and 12 year olds,”, Ophthalmology, vol. 115, no. 4, pp. 678-85, Apr 2008, doi: 10.1016/j.ophtha.2007.04.061.
- D. I. Flitcroft ., “Emmetropisation and the Aetiology of Refractive Errors,” Eye(Lond), vol. 28, no. 2, pp. 169-79, Feb 2014, doi: 10.1038/eye.2013.276
- V. D. Castagno et al., “Hyperopia: a meta -analysis of prevalence and a review of associated factors among school aged children,” BMC Ophthalmology, vol. 14, no. 163, Dec 23 2014.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
