Macular Hole
Macular hole – Written by Dr. Stacy Chan Hsiao Lan, Bachelor of Optometry (N.Z), Doctorate in Optometry (U.K)
What is a macular hole?
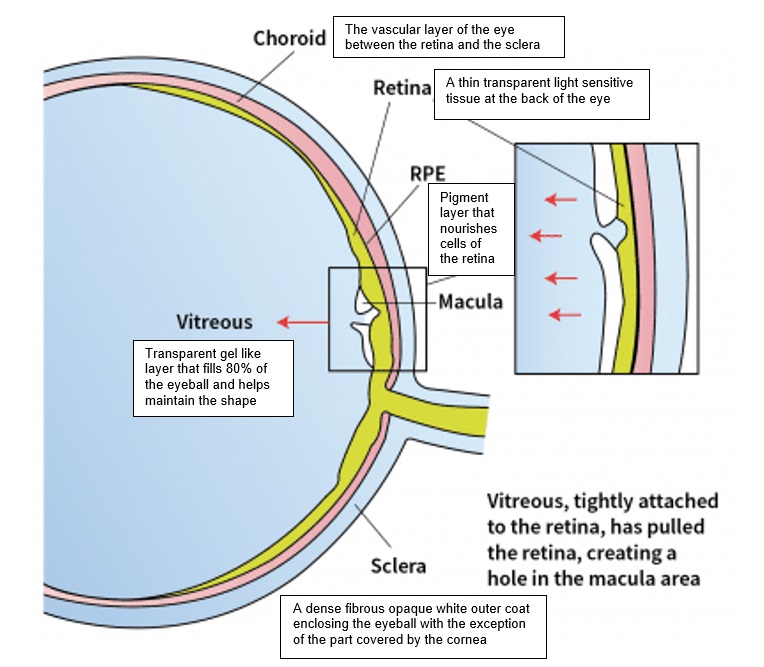
The macula is an area within the retina (a thin transparent, light sensitive tissue at the back of the eye) that is responsible for sharp, central and colour vision. When parts of the macula layer detach from the retina, it’s referred to as a partial macular hole and when all of the macula detaches from the retina, it is referred to as a full thickness macular hole.
The following sections will briefly outline the global problem of the condition, who is at risk, how it develops, its signs and symptoms, its different stages, and some insights into its treatment and prevention options.
The global problem of macular hole
The results of several large-scale population-based studies concluded that the full thickness macular hole (when all of the macula detaches from the retina) occurs in about 3 per 1,000 individuals [1–4]. In the United States of America (Olmsted County), every year the number of new cases of full thickness macular hole is about 8 individuals per 100,000 population [5] and in Australia (Tasmania), the number of new cases each year is about 4 individuals per 100,000 people [6].
Who is at risk of getting a macular hole?
The incidence of macular hole increases with age and it usually affects people above the age of 60 [7], with women having a three times higher risk [8].
Macular hole is one of the complications found in patients with myopia, particularly those with high myopia (prescription greater than -6.00 dioptres) [9-10]. Approximately 1 in 10 people with myopia have the condition [11]. Due to the high prevalence of myopia in the Asian population, the incidence of myopic macular hole is greater in Asians compared to Caucasians or African Americans [8].
What are the common symptoms of a macular hole?
Depending on the stage and severity of the macular hole, vision may be near normal or severely reduced. People with the condition may also notice distortion or a blind spot (an area where vision is obstructed) in their central vision.

If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
What causes a macular hole?
A macular hole can occur due to age, myopia (short sightedness) or by trauma to the eye and these are briefly described in the following section.
Age-related causes
The eye’s interior is filled with vitreous (a transparent gel like substance that fills approximately 80% of the eye and helps maintain a round shape). The vitreous contains millions of delicate fibres that are attached to the surface of the retina (a thin transparent, light sensitive tissue at the back of the eye). With age, the vitreous shrinks and pulls away from the surface of the retina. Natural fluid replaces the area where the vitreous has contracted. When the vitreous pulls away, it can tear the retina and create a macular hole. The fluid that has replaced the vitreous can seep through the hole onto the macula, causing blurry and distorted central vision.

Myopia (shortsightedness)
Macular hole formation in people with myopia can occur in a similar manner as a macular hole formed due to age. For people with progressing myopia, the shape of the eye is constantly undergoing elongation, resulting in the thinning and stretching of each layer of the retina. In addition, this change results in a change of the vitreous, causing contraction and change of state from gel-like to liquid. With this structural change, the macula is prone to schisis (separation of layers), detachment, and holes.
The fovea is a small depression in the centre of the macula, responsible for central vision. Fovea schisis is a common finding in people with high myopia (9 to 34%) [14] and is believed to be one of the main causes of macular hole formation in these patients [15]. With macula schisis and constant traction, it can evolve to a full thickness macular hole [16].

Trauma
Following a blunt trauma or injury, a macular hole may form due to vitreous traction, retinal cell death due to contusion, or due to globe deformation.
Stages of macular hole
There are 3 stages to a macular hole.
Stage 1a: Impending macular hole
An impending macular hole occurs when there is splitting between the inner layers of the retina, forming a cavity.
Stage 1b: Occult macular hole
In this stage, there is a loss of structural support within the inner retinal layers. Reduced and distortion of vision may be noticed in an occult macular hole.
Stage 2: Partial thickness macular hole
The second stage of a macular hole is a partial thickness hole measuring at less than 400 micrometers.
Stage 3: Full thickness macular hole
The third stage of a macular hole is a full thickness hole measuring at more than 400 micrometers. Reduced and distortion of vision progresses in a full thickness macular hole.

How is a macular hole diagnosed?
Vision and amsler grid
Depending on the severity and stage of the macular hole, vision may be normal or severely reduced. In severe cases, people may complain of metamorphopsia (distortion of vision) or central blind spot and this is tested using an amsler grid.

(Source: Researchgate, 2021)
Fundus photography
An image of the retina is taken and a full thickness macular hole is visible in the image.
Optical coherence tomography
An optical coherence tomography (OCT) is a state-of-the-art equipment that provides a high-resolution cross section of the retina and measures the retinal thickness. It is useful in the diagnosis and staging of macular holes and can even measure the volume of a full-thickness macular hole. The information it provides could assist ophthalmologists on the treatment option that is most suitable.

(Source: Advanced Eye Hospital, 2021)
Fluorescein angiography
This test involves injecting a dye into the veins and an eye with a macular hole will reveal a glow in the fovea (small depression in the centre of the macula, responsible for central vision).
How is a macular hole treated?
Visual acuity before surgery is the most important prediction for successful macular hole surgery. The better the visual acuity before the operation is, the higher the rates of visual recovery and hole closure [18]. People with shorter duration of symptoms will also have better visual outcomes as well as closure of macular hole [19].
No treatment is recommended for stage 1a and 1b macular holes as they resolve spontaneously half of the time, but they need to be under close observation [20].
Vitrectomy (removal of vitreous from the eye) is performed for macular holes stage 2 and higher and has been reported to have a high success rate (more than 85%) [21]. The goal of vitrectomy is to release all vitreoretinal tractions from the vitreous and the tissue surrounding the retinal as well as to reduce macula stretching.
Membrane peeling has also become a routine technique for macular hole surgery for most surgeons as it has shown to increase the rate of closure for macular hole [22]. In eyes with a large macular hole or those associated with myopia, the inverted membrane peeling is an alternative surgical technique to internal limiting membrane peeling in order to increase the success rate of macular hole closure. In inverted internal limiting membrane peeling, the remnant of an incomplete internal limiting membrane peeling is left and inverted inside the macular hole to provide a scaffold for macular hole closure.
Following vitrectomy and/or internal limiting membrane peeling, a high surface tension agent such as air, gas, heavy liquids (perfluorocarbons) or silicone oils are introduced into the eye cavity to prevent fluid from entering the hole, further separating the retina layers. In addition, this agent helps retinal cells to migrate to the hole and close it. To increase the efficacy of this agent, the affected person will need to be in a face-down position for 1 to 2 weeks and may be monitored periodically with an OCT scan so that he or she can resume normal position once the OCT image has shown that the macular hole has closed.
In people with high myopia (prescription greater than -6 dioptres), the success rate of vitrectomy varies around 60% and higher [23-24]. Other surgical techniques such as episcleral posterior buckling, suprachoroidal buckling, and scleral shortening technique have been developed for macular hole repair in people with high myopia [25].
Can a macular hole be prevented?
Unfortunately, there are no proven effective methods to prevent a macular hole from occurring and patients are advised to see an optometrist or ophthalmologist immediately if they notice any change, such as blurriness, distortion, or a black patch in their central vision.
In addition, patients are advised to schedule for regular eye examinations as the optometrist or ophthalmologist can test for macular holes and may diagnose one in its earliest stages. With early diagnosis, the chances of visual recovery and hole closure will be higher.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References:
- B. Rahmani et al., “The cause-specific prevalence of visual impairment in an urban population: the Baltimore Eye Survey,” Ophthalmology, vol. 103, no. 11, pp. 1721–1726, 1996.
- P. Mitchell, W. Smith, T. Chey, J. J. Wang, and A. Chang, “Prevalence and associations of epiretinal membranes: the Blue Mountains Eye Study, Australia,” Ophthalmology, vol. 104, no. 6, pp. 1033–1040, 1997.
- [3] S. Wang, L. Xu, and J. B. Jonas, “Prevalence of full-thickness macular holes in urban and rural adult Chinese: the Beijing Eye Study,” Am. J. Ophthalmol., vol. 141, no. 3, pp. 589–591, 2006.
- [4] P. Sen, A. Bhargava, L. Vijaya, and R. George, “Prevalence of idiopathic macular hole in adult rural and urban south Indian population,” Clin. Experiment. Ophthalmol., vol. 36, no. 3, pp. 257–260, 2008.
- [5] C. A. McCannel, J. L. Ensminger, N. N. Diehl, and D. N. Hodge, “Population-based incidence of macular holes,” Ophthalmology, vol. 116, no. 7, pp. 1366–1369, 2009.
- [6] E. Darian‐Smith, A. R. Howie, P. L. Allen, and B. J. Vote, “Tasmanian macular hole study: whole population‐based incidence of full thickness macular hole,” Clin. Experiment. Ophthalmol., vol. 44, no. 9, pp. 812–816, 2016.
- [7] H. A. Madi, I. Masri, and D. H. Steel, “Optimal management of idiopathic macular holes,” Clin. Ophthalmol. Auckl. NZ, vol. 10, p. 97, 2016.
- [8] F. S. Ali, J. D. Stein, T. S. Blachley, S. Ackley, and J. M. Stewart, “Incidence of and risk factors for developing idiopathic macular hole among a diverse group of patients throughout the United States,” JAMA Ophthalmol., vol. 135, no. 4, pp. 299–305, 2017.
- [9] H. Kobayashi, K. Kobayashi, and S. Okinami, “Macular hole and myopic refraction,” Br. J. Ophthalmol., vol. 86, no. 11, pp. 1269–1273, 2002.
- [10] A. Singh, M. Muqit, and W. Woon, “Is axial length a risk factor for idiopathic macular hole formation?,” Int. Ophthalmol., vol. 32, no. 4, pp. 393–396, 2012.
- [11] G. Ripandelli, T. Rossi, F. Scarinci, C. Scassa, V. Parisi, and M. Stirpe, “Macular vitreoretinal interface abnormalities in highly myopic eyes with posterior staphyloma: 5-year follow-up,” Retina, vol. 32, no. 8, pp. 1531–1538, 2012.
- [12] E. Yamada, “Some structural features of the fovea centralis in the human retina,” Arch. Ophthalmol., vol. 82, no. 2, pp. 151–159, 1969.
- [13] R. F. Spaide, “Macular hole hypotheses,” Am. J. Ophthalmol., vol. 139, no. 1, pp. 149–151, 2005.
- [14] M. Alkabes et al., “Anatomical and visual outcomes in high myopic macular hole (HM-MH) without retinal detachment: a review,” Graefes Arch. Clin. Exp. Ophthalmol., vol. 252, no. 2, pp. 191–199, 2014.
- [15] D. Gaucher et al., “Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome,” Am. J. Ophthalmol., vol. 143, no. 3, pp. 455–462, 2007.
- [16] C. Lin, T. Ho, and C. Yang, “The development and evolution of full thickness macular hole in highly myopic eyes,” Eye, vol. 29, no. 3, pp. 388–396, 2015.
- [17] G. Bikbova, T. Oshitari, T. Baba, S. Yamamoto, and K. Mori, “Pathogenesis and management of macular hole: review of current advances,” J. Ophthalmol., vol. 2019, 2019.
- [18] B. Gupta, D. Laidlaw, T. Williamson, S. Shah, R. Wong, and S. Wren, “Predicting visual success in macular hole surgery,” Br. J. Ophthalmol., vol. 93, no. 11, pp. 1488–1491, 2009.
- [19] L. A. Stec, R. D. Ross, G. A. Williams, M. T. Trese, R. R. Margherio, and M. S. Cox Jr, “Vitrectomy for chronic macular holes,” Retina, vol. 24, no. 3, pp. 341–347, 2004.
- [20] H. Oh and Y. Oshima, Microincision vitrectomy surgery: emerging techniques and technology. Karger Medical and Scientific Publishers, 2014.
- [21] L. Wakely, R. Rahman, and J. Stephenson, “A comparison of several methods of macular hole measurement using optical coherence tomography, and their value in predicting anatomical and visual outcomes,” Br. J. Ophthalmol., vol. 96, no. 7, pp. 1003–1007, 2012.
- [22] N. Lois et al., “Internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole: a pragmatic randomized controlled trial,” Invest. Ophthalmol. Vis. Sci., vol. 52, no. 3, pp. 1586–1592, 2011.
- [23] S. Kuriyama, H. Hayashi, Y. Jingami, N. Kuramoto, J. Akita, and M. Matsumoto, “Efficacy of inverted internal limiting membrane flap technique for the treatment of macular hole in high myopia,” Am. J. Ophthalmol., vol. 156, no. 1, pp. 125–131, 2013.
- [24] T.-T. Wu, Y.-H. Kung, C.-Y. Chang, and S.-P. Chang, “Surgical outcomes in eyes with extremely high myopia for macular hole without retinal detachment,” Retina, vol. 38, no. 10, pp. 2051–2055, 2018.
- [25] C. De Giacinto, M. R. Pastore, G. Cirigliano, and D. Tognetto, “Macular hole in myopic eyes: a narrative review of the current surgical techniques,” J. Ophthalmol., vol. 2019, 2019.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
