Ocular Toxoplasmosis
Ocular toxoplasmosis – Written by Associate Professor Lauren Ayton, B Optom, PhD, FAAO, FACO.
What is toxoplasmosis?
Toxoplasmosis is a condition that develops after infection by the toxoplasma gondii parasite. Ocular toxoplasmosis is the term for the effects in the eye of a toxoplasma gondii infection. This parasite is one of the most common in the world. In the USA, it is estimated that around 1 in 10 people over the age of 6 years have been infected at some point in their life.[1] In developing countries, this can be as high as 6 in 10 people.[1]
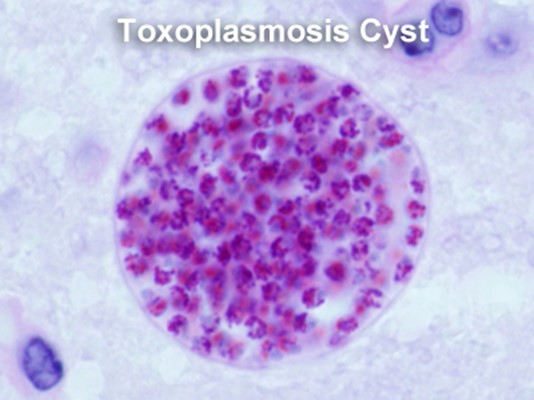
Figure 1. Toxoplasmosis cell
(Source: RVA Retina, 2022)
The following sections will briefly outline how toxoplasmosis develops, its signs and symptoms, and will then dive into ocular toxoplasmosis, its signs and symptoms and treatment options.
How does toxoplasmosis develop?
The toxoplasma gondii parasite is typically acquired in humans through one of three routes:
Food borne
The parasite can be ingested through undercooked meat or shellfish. This can include poor hygiene after touching uncooked meat products (not washing hands properly), or through contaminated cooking or eating utensils.
Animal to human infection
The most common example of animal to human infection is via cats, as they are easily infected with the parasite after eating prey (birds, rodents etc). Infected cats then shed the parasite into their litter box, or outside soil or water, and humans can then acquire it through contact with the faeces or contaminated materials.
Congenital
Pregnant women who are infected with the toxoplasma gondii parasite can pass the infection on to their unborn child, which can lead to severe neurological or ocular damage. Infections in the 3rd trimester are most likely to cause congenital disease. However, early infections in the 1st trimester can lead to more serious outcomes (including seizures, jaundice and ocular toxoplasmosis).
It is very rare for the parasite to be transmitted between adult humans, and usually only happens following blood or tissue transplantation.
Toxoplasmosis is more common in hot and humid locations, as the parasite has a higher survival rate in these conditions.
What are the signs and symptoms of an acute systemic toxoplasmosis infection?
Most people who are infected with toxoplasma gondii are unaware, as humans often do not develop symptoms. In some cases, people may have flu-like symptoms, including headache, fever, body aches and fatigue.
A blood test can be used to determine whether antibodies are present for the toxoplasma gondii parasite, but these tests are unable to distinguish between active and old infections. In pregnant women, the fetus can be tested using an amniocentesis (a procedure used to take out a small sample of the fluid that surrounds the fetus in a pregnant woman).
How is acute toxoplasmosis treated?
Most people do not require treatment for an acute systemic infection. If required, antibiotics and folic acid-blocking drugs can be used.
What are the signs and symptoms of ocular toxoplasmosis?
Ocular toxoplasmosis can either be acquired or congenital. Most patients present with the ocular symptoms of infection in their 2nd to 4th decade of life, and disease is usually more severe in older patients.[2]
In most cases, the initial eye infection from toxoplasma gondii is asymptomatic. However, the parasite may be reactivated at a later stage, leading to:
- Eye pain
- Blurred vision
- Floaters
Ocular toxoplasmosis can be diagnosed by an eye care practitioner, who will complete a comprehensive examination of the retina and optic disc. This may include photographs and scans of the eye. There are a number of conditions which can mimic ocular toxoplasmosis, so it is important that a thorough workup is completed.
The parasite causes inflammation of the back of the eye (called posterior uveitis), and is seen as a fluffy, creamy-white lesion on the retina. After the lesion resolves, a scar is formed, which has a characteristic appearance (Figure 2).

Figure 2. A typical retinal scar following ocular toxoplasmosis, with darkened, pigmented areas.(Source: Dr Jonathan Ruddle)
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is ocular toxoplasmosis treated?
Depending on the individual, an active toxoplasmosis infection may not require treatment and symptoms can resolve over 4 to 8 weeks. However, if there is a chance that vision may be affected, then the infection can be treated with anti-parasitic medications, steroids, and antibiotics.
Of particular note, these treatments do not prevent recurrences, and so the individual should monitor their vision for any changes, and seek regular eye examinations.
Up to 24% of people who have ocular toxoplasmosis may develop legal blindness in the affected eye [3], making regular eye care essential for monitoring and treating the condition.
Can I reduce the risk of developing toxoplasmosis?
Anyone can become infected with the toxoplasma gondii parasite, but the risks are higher if you are pregnant or have immunosuppression (HIV-positive, undergoing chemotherapy or taking immunosuppressant drugs). Whilst all people should limit their risk of toxoplasmosis, these individuals should be particularly careful.
The best way to reduce the risk is to ensure you:
- Don’t eat raw or undercooked meat or shellfish
- Use good hand hygiene at all times, and particularly after cooking or cleaning cat litter
- Wear gloves when you garden or handle soil
- Wash cooking utensils, chopping boards etc. in hot soapy water after every use
- Cover children’s sandpits; cats often use sandpits as an outside litter tray, making it a potential source of infection
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
[1] Centers for Disease Control and Prevention. Parasites – Toxoplasmosis (Toxoplasma infection). www.cdc.gov/parasites/toxoplasmosis 2018.
[2] Dodds EM, Holland GN, Stanford MR, et al. Intraocular inflammation associated with ocular toxoplasmosis: relationships at initial examination. Am J Ophthalmol 2008;146(6):856-65 e2.
[3] Kim SJ, Scott IU, Brown GC, et al. Interventions for toxoplasma retinochoroiditis: a report by the American Academy of Ophthalmology. Ophthalmology 2013;120(2):371-8.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
