Recurrent corneal erosion syndrome (RCES)
Recurrent corneal erosion syndrome (RCES) – Written by Dr Alexis Ceecee Britten-Jones, B Optom (Hons), PhD.
What is recurrent corneal erosion syndrome?
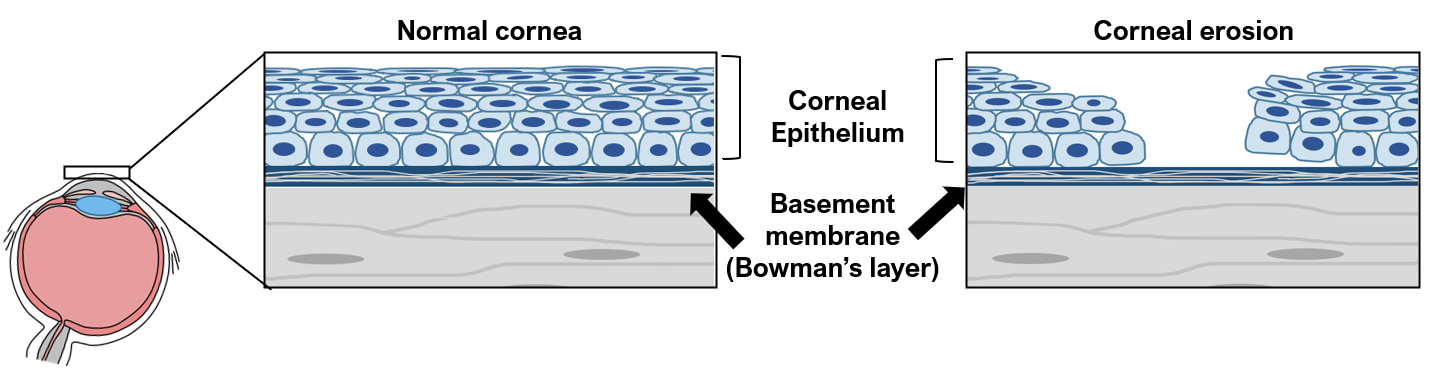
Recurrent corneal erosion syndrome (RCES) is an eye condition where cells in the outermost layer of the cornea, the clear and transparent tissue in the front of the eye, do not adhere properly to the basement membrane underneath (Bowman’s layer).
Symptoms of RCES often occur when the eyes first open in the morning. This is because during sleep, the eyes become dry, and the corneal epithelial cells in the front of the eye can stick to the inside of the upper eyelid. Then, when the eyes open in the morning, the epithelial cells are pulled away from the basement membrane, causing them to detach from the cornea.
RCES is a recurrent condition. This means that even though the symptoms usually get better during the day, it can happen again.
This overview will cover how common is RCES, its causes and how it develops, its common signs and symptoms, how it is diagnosed, as well as its treatment strategies.
How common is recurrent corneal erosion syndrome?
After an abrasion or scratch on the cornea, approximately 10% of people develop RCES [1].
Corneal dystrophies are rare genetic conditions that affect approximately 1 in 2000 people [2]. The most common type of corneal dystrophy that is associated with RCES is epithelial basement membrane dystrophy (EBMD), which is also called map-dot-fingerprint dystrophy. One in 10 people with EBMD develop RCES [3].
What causes recurrent corneal erosion syndrome?
Trauma is the most common cause of RCES, accounting for approximately 50% of RCES cases [3]. Fingernail scratches are the most common type of trauma [4]. Other causes include foreign bodies, mascara wands, tree branches, and paper cuts. RCES may not develop straight away and has been reported to occur from 2 days to 16 years after the trauma event.
Another cause of RCES is corneal dystrophy, which are genetic conditions where abnormal materials accumulate in corneal tissues. These genetic eye conditions account for 20-30% of RCES cases.
People with diabetes also have a higher risk of developing RCES, because the cornea does not heal as quickly after injury in diabetes [5]. RCES can also develop after eye surgery.
How does recurrent corneal erosion syndrome develop?
The epithelial cells in the outermost layer of the cornea normally attach firmly to the basement membrane underneath.
After injury, new epithelial cells grow during the healing process. These new cells may not have attached properly to the basement membrane, meaning that they can lift off easily.
In corneal dystrophies, the growth of abnormal tissues between the tissue layers interferes with the adhesion of the epithelial cells.
During sleep, the dryness of the eyes can cause the corneal epithelial tissues in the front of the eye to stick to the eyelids. Swelling of the epithelial cells at night can also worsen the adhesion. Then, in the morning when the eyes open, the corneal epithelial cells are pulled away from the basement membrane, causing a corneal erosion.
The cornea is the most sensitive part of the body; it is 300-600 times more sensitive than the skin [6]. When the corneal epithelial layer is damaged, the nerve endings in the cornea become exposed, which causes pain and discomfort.
What are the common signs and symptoms of recurrent corneal erosion syndrome?
- Sharp pain in the eye, particularly upon waking
- Sensitivity to light
- Watery eyes
- Redness in the eyes
- Swelling of the eyelids
- Twitching of the eyelids
- Foreign body sensation, feeling like there is something in the eye
- Blurry or cloudy vision
RCES usually affects one eye. However, in people with corneal dystrophies, RCES can affect both eyes.
Pain from RCES can last from minutes to hours. As the cornea heals during the day, the pain usually resides to a feeling of grittiness and discomfort. Even when the pain and discomfort goes away, about one in four cases of RCES can reoccur [7].
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
Different severities of recurrent corneal erosion syndrome
The severity of RCES depends on the size of the epithelium that comes loose from the basement membrane. If the epithelial defect is small, the symptoms may be mild, and the cornea could heal very quickly. However, if the epithelial defect is large, the pain and discomfort can last for several days. It can also lead to a corneal infection.
RCES is not an eye infection. However, the corneal epithelium acts as a barrier to protect the eye. When there is a defect in the corneal epithelial layer, there is a risk of an opportunistic infection. Some signs of eye infection include increased pain/discomfort, blurry vision, sticky discharge, and worsening of symptoms. If this happens, it’s important to seek medical advice as soon as possible.
Another possible complication of RCES is scarring and vision loss from recurring injury to the cornea.
How is recurrent corneal erosion syndrome diagnosed?
RCES is usually diagnosed by an eye health professional based on the results of a comprehensive eye check. This includes a vision test and an assessment of the health of the eyes, particularly of the cornea.
How does an eye health professional confirm that you have recurrent corneal erosion syndrome?
The eye health professional will ask about the symptoms and about your eye and medical history. They will also assess your vision to find out if vision is affected.
The eye health professional will closely examine the cornea using a biomicroscope. This is an instrument that shines an external light onto the eyes and allows the examiner to look at different eye structures under magnification.
The eye health professional may put an ocular dye (such as sodium fluorescein, which is a non-toxic yellow dye) in your eyes. Sodium fluorescein will temporarily stain the damaged epithelial cells on the cornea and show where the area of the defect is.

(Source: EyeRounds.org)
How is recurrent corneal erosion syndrome treated?
The main treatment goals for RCES are to allow the tissue to heal, to establish the adhesion between the epithelial cells and the basement membrane, and to relieve pain. Treatment may be medical, surgical, or both.
Lubricating eye drops
Frequent lubrication with lubricating eye drops, or artificial tear supplements, can help provide comfort and promote corneal healing. To prevent the corneal epithelium from sticking to the eyelid during sleep, a thicker lubricant, such as an ointment or a gel-based eye drop, is usually applied at night.
Other eye drops
If the defect on the eye is large, a topical antibiotic eye drop may be used to prevent an eye infection. An anti-inflammatory eye drop can also be prescribed to reduce inflammation and discomfort.
If there is excess swelling in the eye, a high concentration salt solution may be used to draw the excess liquid from the cornea. The salt solution can reduce the swelling and improve the adhesion of the epithelium.
Bandage contact lenses
A contact lens may be placed over the cornea by an eye health professional to prevent the epithelium from sticking to the lid, to help the cornea heal without interruptions. The contact lens will be a special type that can be left on during sleep. The eye health professional will usually remove the contact lens from the eye once the cornea heals.
Pain relief medications
Pain caused by RCES can be managed using over-the-counter oral pain relief medications, such as paracetamol. It is important to stick to the recommended dosage and to not exceed the maximum daily dose.
Punctal occlusion
In people with dry eye disease, a small plug (punctal plug) may be inserted in the corner of the eyes where the tears normally drain. This treatment, called punctal occlusion, stops the tears in the eyes from draining quickly. This keeps the cornea moist and promotes healing.
Oral antibiotics
A special type of oral antibiotic that has anti-inflammatory effects may be prescribed to reduce the swelling in the eye [8]. This medicine can also help the corneal epithelium adhere to the basement membrane underneath.
Epithelial debridement
An eye health professional may use an instrument to remove loose tissues from the cornea, to allow new healthy epithelial cells to regrow. This will usually be done after putting in an anaesthetic eye drop, which will numb the cornea temporarily.
Surgical management
Phototherapeutic Keratectomy
A laser treatment may be applied to the front of the eyes to break down the adhesions in the tissues. This allows healthy corneal cells to grow and re-attach with stronger adhesions to the basement membrane.
Anterior stromal micro-puncture
In some cases, very small needles may be used to create micro-punctures, or tiny holes, near the injury site. These punctures can help the epithelium adhere better to the basement membrane [9].
Can I prevent recurrent corneal erosion syndrome?
RCES results from poor healing of the tissues in the front of the eye. This happens because corneal epithelial cells continue to become detached. Regular application of lubricating gel or ointment before sleep, to prevent the epithelial cells from sticking to the eyelid, can promote healing and prevent the recurrence of pain episodes. Compliance with lubrication is important to increase the chance of recovery and improvement.
Preventing injury to the cornea can reduce the risk of developing RCES. This can be done by wearing safety glasses or other protective eye wear when there is a risk of injury to the eye (for example, when gardening or working in dusty environments).
Other co-existing ocular surface diseases, such as such as blepharitis or dry eye disease, should be treated to keep the cornea healthy. This improves the healing of the corneal tissues and reduces the risk of developing eye infections.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, including but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- T. Eke, D. A. Morrison, and D. J. Austin, “Recurrent symptoms following traumatic corneal abrasion: Prevalence, severity, and the effect of a simple regimen of prophylaxis,” Eye, vol. 13, no. 3, pp. 345-347, 1999/05/01 1999, doi: 10.1038/eye.1999.87.
- D. C. Musch, L. M. Niziol, J. D. Stein, R. M. Kamyar, and A. Sugar, “Prevalence of corneal dystrophies in the United States: estimates from claims data,” (in eng), Investigative ophthalmology & visual science, vol. 52, no. 9, pp. 6959-6963, 2011, doi: 10.1167/iovs.11-7771.
- J. J. Reidy, M. P. Paulus, and S. Gona, “Recurrent erosions of the cornea: epidemiology and treatment,” (in eng), Cornea, vol. 19, no. 6, pp. 767-71, Nov 2000, doi: 10.1097/00003226-200011000-00001.
- N. Brown and A. Bron, “Recurrent erosion of the cornea,” Br J Ophthalmol, vol. 60, no. 2, p. 84, 1976, doi: 10.1136/bjo.60.2.84.
- R.-L. Jan et al., “Risk of recurrent corneal erosion in patients with diabetes mellitus in Taiwan: a population-based cohort study,” BMJ open, vol. 10, no. 6, p. e035933, 2020, doi: 10.1136/bmjopen-2019-035933.
- M. Millodot and H. Owens, “The influence of age on the fragility of the cornea,” (in eng), Acta Ophthalmol (Copenh), vol. 62, no. 5, pp. 819-24, Oct 1984, doi: 10.1111/j.1755-3768.1984.tb05810.x.
- S. W. Reeves, P. C. Kang, D. F. Zlogar, P. K. Gupta, S. Stinnett, and N. A. Afshari, “Recurrent Corneal Erosion Syndrome: A Study of 364 Episodes,” (in eng), Ophthalmic Surg Lasers Imaging, pp. 1-2, 2010/03// 2010, doi: 10.3928/15428877-20100215-44.
- M. W. Hope-Ross, P. B. Chell, G. N. Kervick, P. J. McDonnell, and H. S. Jones, “Oral tetracycline in the treatment of recurrent corneal erosions,” (in eng), Eye (Lond), vol. 8 ( Pt 4), pp. 384-8, 1994, doi: 10.1038/eye.1994.91.
- N. Avni Zauberman, P. Artornsombudh, U. Elbaz, Y. Goldich, D. S. Rootman, and C. C. Chan, “Anterior stromal puncture for the treatment of recurrent corneal erosion syndrome: patient clinical features and outcomes,” (in eng), Am J Ophthalmol, vol. 157, no. 2, pp. 273-279.e1, Feb 2014, doi: 10.1016/j.ajo.2013.10.005.
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
