Scleritis
Scleritis – Written by Dr. Jia Hui Lee, MBBS (Hons) and A/Prof Elaine Chong, MBBS MEpi PhD Melb, FAMS, FRANZCO.
What is scleritis?
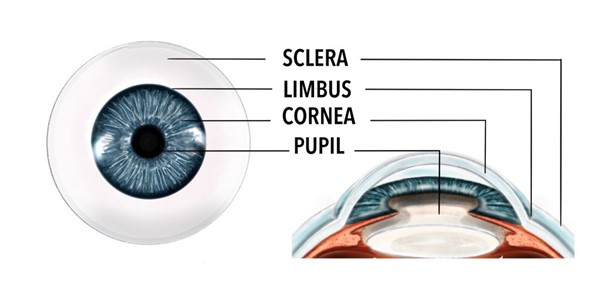
Scleritis refers to inflammation of the sclera, the white part of the eye that lies beneath two thin layers of clear tissue (the conjunctiva and episclera). When the sclera is inflamed, it appears red, swollen, and is usually very painful. Scleritis is a serious condition that if left untreated, can lead to damage to structures of the eye and decreased vision. It is often associated with an underlying systemic autoimmune disease, where the body’s immune system attacks its own tissues, or less commonly, scleritis may be caused by an infection.
The following sections will briefly outline how common is scleritis, what causes scleritis, its signs and symptoms, and some insights into its management.
How common is scleritis?
Scleritis is an uncommon condition. Based on populations in the United States (U.S.) and Australia, studies have estimated that scleritis affects around 1 to 3 per 100 000 people every year [1], [2].
Scleritis typically occurs in middle-aged patients, usually between 4th to 6th decades of life. It is also more common in women [3].
What causes scleritis?
Scleritis can be caused by non-infectious causes, such as systemic autoimmune conditions, surgery, or certain medications. Less commonly, scleritis can be due to infectious causes, such as bacteria, fungi, parasites and viruses. In some cases, there is no known cause.
Non-infectious causes
The most common cause of scleritis is an underlying systemic autoimmune inflammatory disorder, which affects around half of all patients with scleritis. These disorders result when the body’s immune system inappropriately attacks normal tissues and causes inflammation and damage to these tissues. Sometimes, the underlying condition is discovered only after a person develops scleritis. Common systemic autoimmune conditions that are associated with scleritis are [3], [4]:
- Rheumatoid arthritis
- Vasculitis (for example, granulomatosis with polyangiitis)
- Lupus
- Scleroderma
- Sjogren’s syndrome
- Inflammatory bowel disease
Rarely, scleritis can also develop after trauma to the eye or after certain eye surgeries such as pterygium surgery (removal of a fleshy overgrowth on the surface of the eye) or scleral buckle surgery (where a band is attached to the sclera to repair a detached retina) [5].
Certain medications are also known to cause scleritis as a rare side effect, such as bisphosphonates, which are used to treat osteoporosis [3].
Infectious causes
Approximately 5 to 10% of scleritis cases are caused by infections such as bacteria, parasites, fungi and viruses [6]. People with infectious scleritis often have a predisposing factor for the infection. The most common factor is previous ocular surgery, especially pterygium surgery. Other risk factors for infectious scleritis include injury to the eye, use of radiation to the eye, or chemotherapy agents applied to the eye, such as mitomycin [6].
The most common organism identified in infectious scleritis is a bacteria called Pseudomonas aeruginosa. Other bacteria that may cause scleritis include Norcardia, Streptococcus, Haemophilus [6].
Infectious scleritis caused by fungal organisms are usually more aggressive and harder to treat, which can lead to poorer outcomes. Some fungal organisms that cause scleritis include Candida and Aspergillus.
Rarely, infectious scleritis can be caused by parasites, such as Toxoplasma gondii, and viruses such as the varicella zoster and herpes simplex virus [6].
What are the common signs and symptoms of scleritis?
The signs and symptoms of scleritis can vary depending on the type of scleritis. There are two main types of scleritis:
- Anterior scleritis: inflammation of the sclera anterior to or in front of the extraocular muscles (extraocular muscles control eye movement and alignment)
- Posterior scleritis: inflammation of the sclera posterior to or behind the insertion of the extraocular muscles
Anterior scleritis is more common and accounts for 98% of scleritis cases [3]. Anterior scleritis may be further classified into the following subtypes [3]:
- Diffuse – where the inflammation and redness affects either a sector or the entire sclera
- Nodular – where there are well defined, non-mobile nodules (a raised bump) formed on the sclera
- Necrotising – where there is thinning of the sclera leading to possible exposure of the inner contents of the eye. This is the most severe form of anterior scleritis with the worst prognosis.

In cases of anterior scleritis, the person affected may have the following symptoms and signs:
- Severe boring eye pain – the pain may wake the person up at night and may be worse with eye movements
- Redness of the eye – usually a darker red described as a violet-bluish hue
- Swelling of the white part of the eye
- Sensitivity to light
- Excessive tearing
- Blurred vision
Posterior scleritis is rarer, and because it affects the back of the eye which is not externally visible, it is often more difficult to diagnose. People with posterior scleritis may not have any eye redness, pain, or any noticeable signs at the front of the eye. However, in some cases, people with posterior scleritis may also experience some of the above symptoms and signs that occur with anterior scleritis.
If you experience any of these signs and symptoms, schedule an appointment with an eye health professional to get your eyes checked. It is also important to note that the development of eye conditions may even start before symptoms appear, which makes going for regular and timely eye checks that much more essential.
How is scleritis diagnosed?
Scleritis is usually diagnosed by an eye care professional based on a comprehensive eye check. This includes a vision test, a slit lamp examination (a microscope used to look at eye structures under high magnification in detail), and may also encompass some scans and photos of the back of the eye.
In anterior scleritis, a slit lamp examination should reveal a blue-violet dark red hue of deep inflamed blood vessels on the white of the eye. This is in contrast to episcleritis or conjunctivitis, where the inflammation of blood vessels is superficial and appears a lighter or brighter red. Often, it can be difficult to see which layer of vessels on the eye is inflamed. An eye drop called phenylephrine can be used to help further distinguish this and differentiate scleritis from other conditions that also cause a red eye (for example, episcleritis).
In scleritis, the phenylephrine eye drop will not cause any blanching of the deeper inflamed blood vessels, and thus the eye should still look a deep red colour even after instillation of the eye drop. In contrast, in episcleritis, the superficial inflamed blood vessels will blanch 10 to 15 minutes after instillation of the phenylephrine eye drop, and the eye will look less red [3].
There are some additional signs that may be seen in certain subtypes of scleritis. In nodular scleritis, there may be one or multiple raised, non-mobile bumps that are a deep violet colour located on the sclera. In necrotising scleritis, there is thinning of the sclera, and exposure of the inner ocular contents may be visible, which usually appears as a dark brown colour.
In posterior scleritis, a slit lamp examination may not reveal any signs on the front of the eye. An eye care professional may administer eye drops to dilate the patient’s pupil, allowing them to see the back of the patient’s eye (fundus) with a special lens or equipment. In posterior scleritis, a fundus exam may reveal swelling of the optic nerve, or retinal detachments (where the retina, the film responsible for sensing light and receiving visual images, is lifted from its normal position). Vision may also be decreased as a result of this. Additionally, a B-scan ultrasonography (ultrasound of the eye), may reveal a characteristic sign where there is thickening of the sclera and fluid around the optic nerve [3].
As scleritis is often associated with an underlying systemic inflammatory condition, an eye care professional will often order further tests including blood tests and imaging when a person is diagnosed with scleritis. These tests help to identify the underlying inflammatory condition which may be the root cause for the scleritis.
If the scleritis is thought be due to an infectious cause, the eye care professional may also take a small sample of inflamed sclera to send off to the laboratory, in order to identify the organism that is causing the scleritis.
How is scleritis treated?
The treatment of scleritis depends on the underlying cause of the scleritis, the type of scleritis, and the degree of severity of the scleritis.
Non-infectious scleritis
In cases of non-infectious causes of mild to moderate scleritis, oral non-steroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, may be prescribed by an eye care professional. Sometimes, steroid eye drops may also be prescribed to treat these cases.
If the scleritis is severe, necrotising, or is associated with an underlying systemic disease, then the eye care professional will often prescribe high dose oral steroid medication as the first line treatment. In extremely severe cases, high dose steroids may also be given intravenously.
In addition, people with an underlying autoimmune or inflammatory condition will also be referred to a rheumatologist or physician for consideration of a long-term immunosuppressive medication. These medications are required to help prevent recurrences of scleritis, control inflammatory disease elsewhere in the body, and reduce the need for long-term steroid use, which can cause unwanted side effects in the body [3].
Infectious scleritis
In cases of infectious scleritis, treatment is with anti-microbial medications. The specific anti-microbial agent will depend on the type of organism that is causing the scleritis (for example, bacteria, virus, or fungal). The anti-microbial medication may also be delivered in different forms, including as an eye drop, orally as a tablet, or intravenously.
How does scleritis progress?
In cases of mild to moderate scleritis that responds well to treatment, the visual prognosis is usually good. In more severe forms of scleritis, such as necrotising or posterior scleritis, the condition may be more difficult to treat, and there is a higher risk of damage to eye structures which can have long-term impacts on vision [3]. Ultimately, the outcome of treatment depends on the severity of scleritis, the duration of the disease, and if there is an underlying associated systemic autoimmune condition.
Can scleritis be prevented?
In cases of scleritis that are associated with an underlying systemic autoimmune condition, further recurrences of scleritis can be prevented by treating the underlying condition. The treatment of the underlying condition is performed in conjunction with a rheumatologist or physician, and usually consists of a long-term immunosuppressive medication that is taken as an oral tablet, an injection or an intravenous infusion.
DISCLAIMER: THIS WEBSITE DOES NOT PROVIDE MEDICAL ADVICE
The information, include but not limited to, text, graphics, images and other material contained on this website are for informational purposes only. No material on this site is intended to be a substitute for professional medical advice, diagnosis or treatment. Always seek the advice of your physician or other qualified health care provider with any questions you may have regarding a medical condition or treatment and before undertaking a new healthcare regimen, and never disregard professional medical advice or delay in seeking it because of something you have read on this website.
References
- G. Honik, I. G. Wong, and D. C. Gritz, “Incidence and prevalence of episcleritis and scleritis in Northern California,” Cornea, vol. 32, no. 12, pp. 1562–6, 2013, doi: 10.1097/ICO.0b013e3182a407c3.
- L. P. Thong, S. L. Rogers, C. T. Hart, A. J. Hall, and L. L. Lim, “Epidemiology of episcleritis and scleritis in urban Australia,” Clinical & Experimental Ophthalmology, vol. 48, no. 6, pp. 757–766, May 2020, doi: 10.1111/ceo.13761.
- A. Lagina and K. Ramphul, “Scleritis,” PubMed, 2020. https://www.ncbi.nlm.nih.gov/books/NBK499944/.
- J. Daniel Diaz, E. K. Sobol, and D. C. Gritz, “Treatment and management of scleral disorders,” Survey of ophthalmology, vol. 61, no. 6, pp. 702–717, 2016, doi: 10.1016/j.survophthal.2016.06.002.
- R. R. Doshi, G. J. Harocopos, I. R. Schwab, and E. T. Cunningham, “The spectrum of postoperative scleral necrosis,” Survey of Ophthalmology, vol. 58, no. 6, pp. 620–633, Nov. 2013, doi: 10.1016/j.survophthal.2012.11.002.
- M. Moshirfar and Y. Ronquillo, “Infectious Scleritis,” PubMed, 2022. https://www.ncbi.nlm.nih.gov/books/NBK560818/ (accessed Jan. 02, 2022).
Tools Designed for Healthier Eyes
Explore our specifically designed products and services backed by eye health professionals to help keep your children safe online and their eyes healthy.
